Inside This section
Hip Arthroscopy
Hip Arthroscopy is a relatively simple procedure whereby common disorders of the hip can be diagnosed and treated using keyhole surgery. Some conditions, which previously were not treated or required major open surgery, can now be performed using this technique. It is a useful diagnostic tool in investigation of hip pain.

Instruments and camera used

Typical setup for Hip Arthroscopy
Hip Anatomy
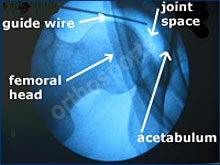
Intraoperative x-ray used to help positioning of the arthroscope in the joint
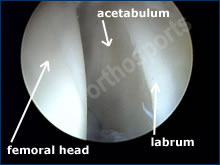
The hip joint is composed of a ball and socket joint. The femoral head (ball) is the top of the femur (thigh bone) and the acetabulum (part of the pelvis) is the socket. These surfaces are both covered by articular cartilage, which is a specialised lining allowing smooth pain free motion of the joint. Damage to this lining results in arthritis.
The joint is lined by a specialised synovial layer, which secretes fluid helping with lubrication. Inflammation of this layer is called inflammatory arthritis the most common of which is rheumatoid arthritis.
The labrum is a specialised structure adding to stability of the joint. Damage to this structure can result in catching and pain in the joint. The capsule surrounds the synovium stabilising the joint.
Indications

Loose body floating in hip joint

Tear of the labrum
- Labral tears
- Removal of loose bodies
- Biopsy of lesions
- Synovectomy
- Diagnosis of pain
- Infection
Contraindications
- Advanced arthritis
- Stiff hip
- Heterotopic ossification
- Severe dysplasia
Pre-Op Instructions
- Cease aspirin and anti-inflammatory medications (e.g. voltaren, feldene) 10 days prior to surgery as they can cause bleeding.
- Cease any naturopathic medications as they can also cause bleeding.
- Continue with all other medications unless otherwise specified.
- Notify me if you have any abrasions or pimples around the hip.
- Please bring any x-rays, MRI scans or other investigations you have had done which may be relevant to your surgery.
- Bring a list of medications with you to give to the anaesthetist.
- You are advised to stop smoking for as long as possible prior to surgery.
Procedure
- Under anaesthetic you are positioned on a special operating table with your legs strapped into boots to allow traction to be placed on the hip. X-ray control is then used to mark out the landmarks used for surgery.
- Specially made instruments are inserted into the hip joint. Two or three small incisions 1 –2 centimeters long are made in the skin during the procedure.
- The first incision is used to insert a camera which displays the inside of the hip on a television monitor and the other incisions are to insert instruments for treatment of the problem.
- Following the procedure local anaesthetic is injected into the hip and wound and the wounds are stitched closed.
- You will usually be in hospital overnight for antibiotics and pain relief.
- Crutches are generally used for a week or so depending on what you have had done.
Post-Op
- Your dressing will be reduced prior to your discharge.
- You will go home the same day or stay one night.
- A physiotherapist will see you before you are discharged and show you how to use crutches. Crutches are generally used for a few days.
- You will be given an appointment to be seen in the rooms in approximately 7 –10 days after the surgery to check the wound and discuss the findings of the operation and any follow up care that may be needed.
- You should be able to drive after one or two weeks depending on your recovery.
- Time off work depends on your occupation usually one to four weeks.
Any operation big or small has risks. The following can occur with any surgery and some rarer complications may also be possible. It is impossible to discuss every complication and there will be some, which no surgeon may anticipate or may never have heard of.
The utmost care is taken at all times during surgery to prevent these complications. At Orthosports we are all subspecialised and operate within our defined area of expertise. We believe this minimises the risk of complications.
The following list is not exhaustive and some are explained in more detail in the various sections to which they may be more appropriate.
Surgical Complications
All of these complications are rare but you need to be aware of them prior to your surgery.
Infection
Infection is rare and can be superficial (skin) or deep (in the hip). If you have any redness around the wound or if you have any temperatures or are feeling unwell you need to contact me as soon as possible. If infection occurs you may require antibiotics either as an outpatient or in hospital. If the infection is deep you may require the hip to be washed out.
Nerve Damage
There are a number of nerves surrounding the hip joint supplying sensation and muscles in the leg. There can be damage to superficial nerves, which can result in temporary or rarely permanent loss of sensation in the groin, thigh, scrotal or labial region.
This can be a result of pressure during the procedure or damage with the insertion of instruments. There can be damage to nerves supplying the muscles of the leg resulting in weakness. This is however very rare.
Vascular Injury
This can result in excess bleeding. Bleeding into the joint or soft tissue may require drainage.
Failure to Relieve Pain
Failure to relieve pain is not common but unfortunately some operations may not be entirely successful in relieving pain.
Allergic Reactions
Allergic reactions to medications or materials used in the operating room.
Thromboembolic Problems
These refer to blood clot formation in the blood vessels of the legs. They usually occur in the leg veins where they are known as deep venous thrombosis (DVT). They cause pain and swelling in the leg due to restriction of blood flow back to the heart. These may require blood thinning medication in the form of injections or tablets.
Occasionally these clots can travel to the lung causing what is called a pulmonary embolus. This can require hospitalisation and can be life threatening. If you get increasing calf pain or shortness of breath you should notify your doctor straight away.
The chance of this complication is higher in bigger operations such as Joint Replacement but may occur with the most minor of procedures, in fact they can occur without surgery at all.
They are more common in smokers, people with obesity and those on the contraceptive pill. Long airplane flights can also cause DVT and flying should be avoided for 2 weeks following surgery. Clots in the arterial system can cause strokes.
Wound Breakdown
This occurs when small areas of the wound may not heal and may need to be resutured. This can sometimes result from reaction to the sutures just under the skin.
Instrument Breakage
Unsightly or Thickened Scar
Joint Stiffness
Joint stiffness can occur no matter what the procedure, this is minimised and treated with physiotherapy.
Reflex Sympathetic Dystrophy
This is an unexplained condition where nerves become hyperactive and the limb painful. This may occur following minor trauma or surgery. This usually but not always resolves over time but may require referral to a specialised pain clinic.
Pressure
Pressure on areas of the body in the operating theatre causing nerve damage.
Diathermy Burns
Diathermy Burns from cautery device used in most open operations (very rare).
Limp
Limp can occur from muscle weakness.
Other Medical Complications
Any other medical complication you have heard about can occur especially if you already have a pre-existing medical problem. Such complications include heart attack, stroke, kidney failure, pneumonia, bowel obstruction, bladder infection or obstruction etc. Serious medical problems can lead to ongoing health concerns, prolonged hospitalisation or rarely death.
Conclusion
Hip arthroscopy is a procedure useful for relieving pain from a number of hip conditions. It is a relatively small procedure performed through small skin incisions. The complication rate is low but prior to your procedure you must be aware of these risks. If you have any further questions please ask before surgery
