Welcome to Orthosports Question for Physiotherapists August 2025. This month Dr Kwan Yeoh discusses wrist fractures and xrays.
REGISTRATIONS OPEN Orthosports Annual Orthopaedic Updates, Saturday, 8th November, 2025, to register for the live event @UNSW CLICK HERE or to register for the webinar CLICK HERE
If you have a Question that you would like answered on this monthly email please send to education@orthosports.com.au

QUESTION | I have a patient who fell while snowboarding with a wrist fracture about 7 weeks ago. The most recent x-ray report says that the fracture hasn’t healed and the patient is being referred to a surgeon.
Is an x-ray necessary when the patient comes out of the cast if the fracture isn’t sore?
When should we be getting x-rays of a patient’s fracture?
ANSWER | I’ll break my answer down into the two questions that have been asked:
Is an x-ray necessary when the patient comes out of the cast if the fracture isn’t sore? This is something that I see commonly, where a patient is referred to me at around 6–8 weeks because the radiology report says that the fracture hasn’t healed, which, in your example, is most likely a distal radius fracture. Snowboarding patients are largely younger and fitter, and the fracture site is probably no longer tender. However, the patient will come in quite concerned about the x-ray report and the reason for the referral to me.
In general terms, fractures heal clinically and structurally before healing is seen radiologically. Therefore, it is generally safe to get a patient moving before full radiological union is demonstrated if the fracture is not tender to palpation at the expected time frame. Because the strength of a fracture site increases gradually, start with just range of motion, then progress to strengthening later. Sudden impact forces and sports may need even a little more time.
Distal radius fractures usually need about 6 weeks to heal sufficiently to start moving. Careful palpation will reveal whether the fracture site is tender or not—caution needs to be exercised to distinguish between fracture site tenderness, joint tenderness or a potential missed fracture at a different site nearby. An x-ray taken at this time serves to check the position in which the bone is healing, rather than to check for bony union itself. Once I start a patient moving out of the cast, I would usually not perform any further x-rays to check for radiological union unless the patient had any ongoing problems.
However, there are some exceptions where I would definitely want to see radiological union before mobilising, the most notable of which is a scaphoid waist fracture. These injuries often have very little pain or tenderness despite not having healed, so judging healing by palpation alone is fraught with danger. Furthermore, the consequences of getting this fracture moving before it has healed can be disastrous, with future displacement, non-union, avascular necrosis and a terrible outcome. Therefore, I always ensure I have radiological and clinical union before moving a scaphoid waist fracture patient. Depending on the patient and the fracture pattern, I may be happy to use x-ray alone, but I will request a CT scan if I am unsure.
When should we be getting x-rays of a patient’s fracture? To your second question, let’s take an example of a patient who is being seen within a day or two of the injury. Let’s assume the fracture pattern is acceptable for non-operative management via immobilisation—a distal radius fracture, an olecranon fracture, a metacarpal fracture, or so on. At this time, a judgement call needs to be made as to the fracture stability.
If the fracture has a stable pattern with a low risk of displacement, and if potential displacement is unlikely to lead to dire outcomes, then it might be okay to avoid any further x-rays until starting to mobilise.
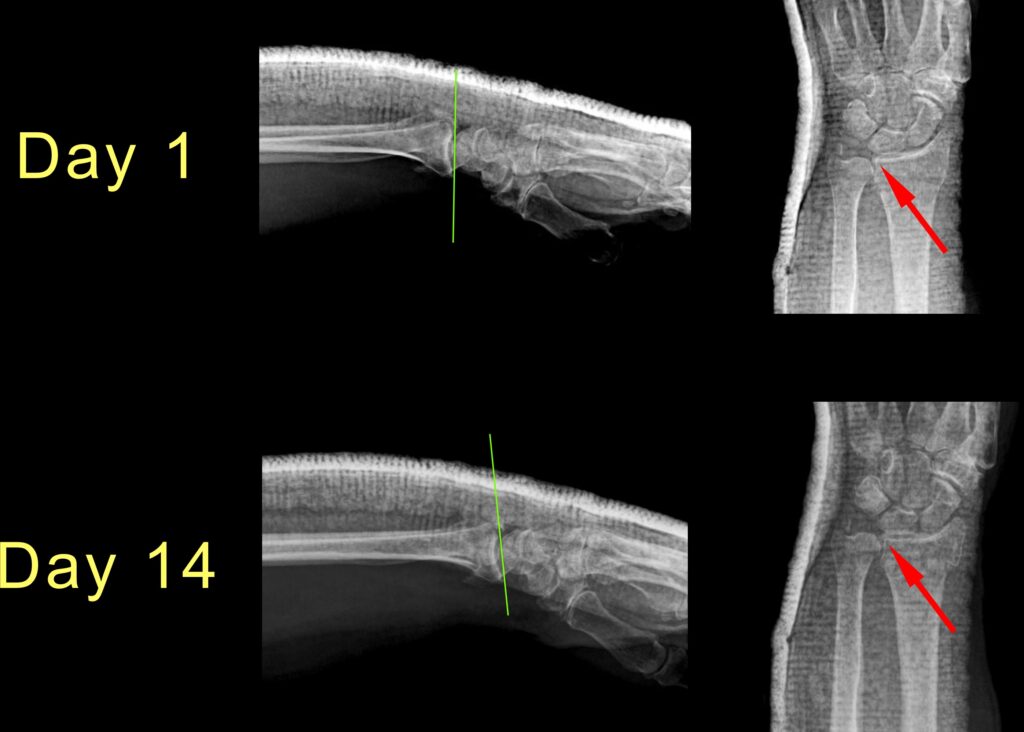
However, if the fracture has an unstable pattern with a higher risk of displacement, or if any displacement is likely to lead to worse longer-term outcomes, then progress x-rays should be made in the first couple of weeks. The purpose of these x-rays would be to detect fracture displacement early enough that correction and fixation could be performed while the fracture is still mobile.
As a general principle—but modified depending on the actual fracture—after my initial Day 0 x-ray, I would get another x-ray at around Day 7 and another at around Day 14. By this time, the fracture is usually starting to heal sufficiently that it is unlikely to displace any further, but this would once again depend upon a judgement call on the nature of the injury.
I would then have another x-ray done to document final healing position at the time of starting to mobilise.