QUESTION | WHEN DOES A COLLATERAL LIGAMENT TEAR OF THE THUMB NEED SURGERY?
ANSWER | For the purposes of this question, I’m going to assume it relates to the MCP joint of the thumb, as this is the joint where the collateral ligament is usually injured. The collateral ligaments of the IP joint are much more uncommonly injured.
The most common injury to a collateral ligament at the MCP joint of the thumb is a skiers’ thumb. This is a tear of the ulnar collateral ligament (UCL) which occurs when the thumb is forcefully pushed into radial deviation. Classically, this could be due to a ski pole during a fall. Usually, the ligament fails at its distal attachment into the base of the proximal phalanx.
Partial tears are usually treated non-operatively with a splint for about 4-6 weeks, whereas complete tears may be treated operatively or non-operatively. The decision as to which path to take depends on the assessed likelihood of the ligament healing
with immobilisation alone. Generally, the closer the ruptured end of the ligament lies to its native attachment site, the higher the chance of successful healing without surgery.
The initial assessment of a patient’s thumb is a careful history of the direction of applied force. Careful palpation will then isolate the site of injury to the UCL, with the tenderness usually at the attachment site into the proximal phalanx. However, if the ligament has folded back upon itself, then the tender spot may be more proximal, where the end of the ligament now lies.
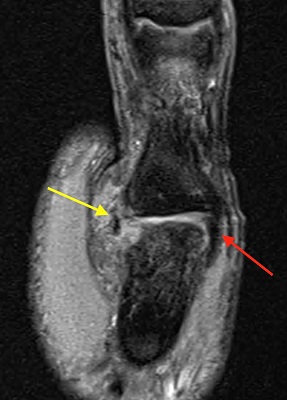
At this stage, I would arrange an x-ray of the joint as an avulsion fracture would give the diagnosis immediately. If the fracture fragment is sitting in the anatomical position, then we would not want to displace it by passively radially deviating the joint in a stability test. A markedly displaced avulsion fragment would need surgical reduction and fixation as the bone fragment and ligament end may have displaced to the wrong side of the overlying adductor aponeurosis and be separated from where it needs to heal to by the aponeurosis. This displacement is known as a Stener lesion and should be operated on as soon as possible before the ligament scars in its displaced position and becomes unrepairable.
If there is no fracture, then the next step is to assess joint stability by passively radially deviating the joint. If there is increased laxity compared to the contralateral thumb, perhaps without a solid endpoint to the force, then this would indicate UCL laxity and most likely a tear. An ultrasound or MRI at this stage will determine whether the tear is complete or partial. If a complete tear, it would also show if the ligament is displaced as a Stener lesion. Once again, a Stener lesion requires surgery. A complete tear with an unstable joint that opens into radial deviation more than the contralateral thumb should also be treated operatively. Non-displaced complete tears and partial tears with a stable joint can be treated non-operatively with immobilisation and rehabilitation.
Surgery may also be required if a partial or complete UCL tear continues to have pain despite non-operative treatment as the tear may still not heal. Generally, a decision would be made at around 3 months from injury after immobilisation and attempted rehabilitation.
The radial collateral ligament (RCL) can also be injured at this joint, in this instance due to a forced ulnar deviation. A similar principle applies when assessing for an RCL injury in terms of clinical examination, x-ray and ultrasound/MRI. However, a smaller amount of displacement of the RCL’s distal attachment (whether with an avulsion fracture or without) seems to give a poor outcome when treated nonoperatively, compared to a UCL injury. The periosteum and other soft tissues on the radial side seem to intervene between the disrupted ligament and the required native attachment site, leading to an injury that fails to heal and gives ongoing pain. Therefore, I would generally offer surgery with even a 1mm displacement of an avulsion fracture of the RCL whereas I would treat a 1mm displacement nonoperatively for the UCL.
For the purposes of this question, I’m going to assume it relates to the MCP joint of the thumb, as this is the joint where the collateral ligament is usually injured.
The collateral ligaments of the IP joint are much more uncommonly injured. The most common injury to a collateral ligament at the MCP joint of the thumb is a skiers’ thumb. This is a tear of the ulnar collateral ligament (UCL) which occurs when the thumb is forcefully pushed into radial deviation. Classically, this could be due to a ski pole during a fall. Usually, the ligament fails at its distal attachment into the base of the proximal phalanx. Partial tears are usually treated non-operatively with a splint for about 4-6 weeks, whereas complete tears may be treated operatively or non-operatively. The decision as to which path to take depends on the assessed likelihood of the ligament healing with immobilisation alone. Generally, the closer the ruptured end of the ligament lies to its native attachment site, the higher the chance of successful healing without surgery.
The initial assessment of a patient’s thumb is a careful history of the direction of applied force. Careful palpation will then isolate the site of injury to the UCL, with the tenderness usually at the attachment site into the proximal phalanx. However, if the ligament has folded back upon itself, then the tender spot may be more proximal, where the end of the ligament now lies.
At this stage, I would arrange an x-ray of the joint as an avulsion fracture would give the diagnosis immediately. If the fracture fragment is sitting in the anatomical position, then we would not want to displace it by passively radially deviating the joint in a stability test. A markedly displaced avulsion fragment would need surgical reduction and fixation as the bone fragment and ligament end may have displaced to the wrong side of the overlying adductor aponeurosis and be separated from where it needs to heal to by the aponeurosis. This displacement is known as a Stener lesion and should be operated on as soon as possible before the ligament scars in its displaced position and becomes unrepairable.
If there is no fracture, then the next step is to assess joint stability by passively radially deviating the joint. If there is increased laxity compared to the contralateral thumb, perhaps without a solid endpoint to the force, then this would indicate UCL laxity and most likely a tear. An ultrasound or MRI at this stage will determine whether the tear is complete or partial. If a complete tear, it would also show if the ligament is displaced as a Stener lesion. Once again, a Stener lesion requires surgery. A complete tear with an unstable joint that opens into radial deviation more than the contralateral thumb should also be treated operatively. Non-displaced complete tears and partial tears with a stable joint can be treated non-operatively with immobilisation and rehabilitation.
Surgery may also be required if a partial or complete UCL tear continues to have pain despite non-operative treatment as the tear may still not heal. Generally, a decision would be made at around 3 months from injury after immobilisation and attempted rehabilitation.
The radial collateral ligament (RCL) can also be injured at this joint, in this instance due to a forced ulnar deviation. A similar principle applies when assessing for an RCL injury in terms of clinical examination, x-ray and ultrasound/MRI. However, a smaller amount of displacement of the RCL’s distal attachment (whether with an avulsion fracture or without) seems to give a poor outcome when treated nonoperatively, compared to a UCL injury. The periosteum and other soft tissues on the radial side seem to intervene between the disrupted ligament and the required native attachment site, leading to an injury that fails to heal and gives ongoing pain. Therefore, I would generally offer surgery with even a 1mm displacement of an avulsion fracture of the RCL whereas I would treat a 1mm displacement nonoperatively for the UCL.
Dr Kwan Yeoh

