QUESTION| How Does a Wrist Ganglion relate to Carpal Instability? How is it best treated?
ANSWER | A ganglion is a benign synovium-lined cystic collection of fluid which arises from an adjacent area of injury. Although we may not know the exact mechanism of formation, the area of injury forms a ganglion which then expands out towards a region of least resistance, usually towards the skin. Sometimes, these are flat, sessile structures only found on ultrasound or MRI scan, while other times they are more like a balloon with a long stalk bulging out at the skin surface and noticeable by the patient.
In most cases, the ganglion itself is not painful, but the pain rather comes from the same underlying cause of injury which has caused the ganglion itself. Occasionally, we do find that the local pressure from the ganglion does cause pain in its own right.
In the context of carpal instability, a ganglion may result from a ligament tear or sprain, or as a result of degenerative change associated with ongoing carpal instability. A ganglion would not be the cause of carpal instability. Similarly, as described above, a ganglion is unlikely to be the cause of pain itself, but rather pointed to an underlying problem with dynamic or static carpal instability.
The most common dorsal wrist ganglion arises from the scapholunate ligament. This is usually a partial tear arising from chronic overuse or an acute injury. Sometimes, the acute injury itself goes untreated as it is thought to be a simple sprain. Ganglions on the volar side of the wrist often arise from the radiocarpal joint itself, from the base of the thumb or from the flexor tendons.
The first step in managing a ganglion is always taking a history from the patient. What is it that the patient is actually complaining of? Is it concern over what this lump is? Is it the cosmetic appearance? Are they experiencing pain and if so, what activities are affected? You may find that the patient just requires simple reassurance, or perhaps further treatment may be necessary.
On palpation, you may find that the ganglion is anywhere from soft and spongy through to quite firm and tense. Try to determine whether the ganglion itself is tender, or perhaps a directly adjacent anatomical structure, such as the scapholunate ligament.
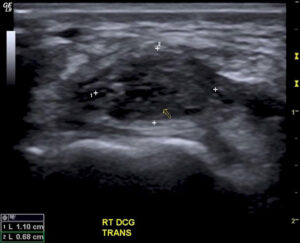
A plain wrist x-ray and an ultrasound (or MRI) would be useful investigations in guiding treatment. Together, these will show overall wrist and carpal bone alignment, reveal any underlying degenerative change, and look for any acute or previous fracture which may contribute to the pain. They would also confirm the lump as a ganglion rather than another type of pathology.
Treatment
In determining the best treatment, ensure that the patient understands that the ganglion arises from an underlying abnormality which is the more likely cause of pain or discomfort. Therefore, eradicating the ganglion itself doesn’t necessarily mean that the pain will subside.
Some ganglions will subside spontaneously over time. However, if the patient wishes treatment, then most wrist ganglions can initially be treated with aspiration and a steroid injection (as long as the underlying cause is not one that needs immediate treatment in its own right). The recurrence rate of a ganglion aspiration is above 50%, but it is a relatively simple procedure with low morbidity so is appropriate as a first step in treatment. The steroid injection reduces inflammation and pain from the underlying structural abnormality and reduces the risk of recurrence. Coupling this with targeted exercises will help the patient recover strength and function.
If there is significant pain or reoccurrence despite aspiration and injection, surgery may be warranted. Abnormalities found clinically or seen on plain x-ray, such as abnormal carpal alignment, warrant early referral to a surgeon as it is sometimes better that these are corrected.
Surgery is aimed at removing the whole ganglion, including the synovial sac and its stalk. The underlying cause of the ganglion, such as a joint capsule or ligament, is addressed at the same time by debridement or repair. There is still a recurrence rate after surgery of about 15%.
Surgery can be done as a day only procedure and the patient is usually back to full activities and sports within a couple of months.

