Inside This section
ACL Reconstruction
Introduction
The anterior cruciate ligament (ACL) is one of the major stabilising ligaments in the knee. It is a strong rope like structure located in the centre of the knee running from the femur to the tibia.
The anterior cruciate ligament prevents the femur moving forward and rotating abnormally on the tibia. The ACL is required for normal function of the knee. One of the main functions of the ACL is to provide stability during rotational movements such as turning, twisting and sidestepping.
When it ruptures it does not heal itself and the knee often becomes unstable or gives way. Repeated giving way can lead to damage to other structures of the knee and eventually arthritis. Since the knee ‘dislocates’ when the ligament ruptures there is often damage to other structures in the knee such as bone, cartilage or meniscus. These injuries may also need to be addressed at the time of surgery.
History Of Injury
Usually there is a significant injury involving a twisting force to the knee. It can also occur after landing from a jump, stopping rapidly or direct contact such as in a tackle. It is particularly common in sports such as football, soccer, basketball, netball and skiing but can occur in many other activities.
When the ACL ruptures the patient often feels something giving way in the knee or hear a popping sound. Most people cannot continue with their activity and the knee generally swells up within hours.
Initial Management
The knee should be treated with ice, elevation and a compressive bandage .Crutches and analgesics usually are required. An X-ray is necessary to exclude an associated fracture. Physiotherapy is helpful to reduce swelling and regain motion.
Most patients will be referred to an orthopaedic surgeon for diagnosis and assessment of the injury. Careful clinical examination is required to detect damage to the ACL, other ligaments and structures in the knee such as the meniscus or articular cartilage. It is quite common to damage some of these other structures.
Diagnosis
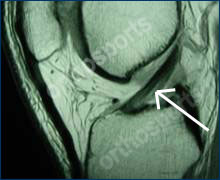
This can usually be made on history and clinical examination. An MRI scan which is a special imaging test is often ordered to confirm the diagnosis in patients where the examination is not conclusive. It also demonstrates damage to other structures such as the menisci or articular cartilage. The diagnosis can also be made with an arthroscopy.
MRI-Scan Normal Cruciate Ligament

Ruptured Cruciate Ligament
To view an animation of ACL Reconstruction see the video below
ACL Reconstruction (Patellar Tendon Graft Technique)
To view an operative video of ACL Reconstruction , click here.
Treatment Recommendations
Most patients who tear their ACL during sport will elect to have it surgically reconstructed, to enable them to return to full activities with a stable knee. Other patients choose to modify their activities and give up sport to avoid further episodes of instability.
In general, the younger and more active you are then the stronger the recommendation for reconstruction. It is generally recommended to have surgery if you wish to get back to sports which involve twisting and pivoting. Many patients who do not have surgery find that their knee becomes more loose over time. This can lead to a knee that gives way during ordinary activities of daily living. These patients should strongly consider surgery to stabilise the knee.
Repeated instability or abnormal movement in the knee can cause ongoing damage leading to stretching of other structures around the knee, meniscal tears or arthritis in the long term. If you do not elect to have surgery it is strongly advised that you give up sports that involve pivoting, sidestepping or rotation.

Typical Setup for Arthroscopic Surgery
Pre-Op Instructions
- Cease aspirin and anti-inflammatory medications (e.g., voltaren, feldene) 10 days prior to surgery as they can cause bleeding.
- Cease any naturopathic or herbal medications 10 days before surgery as these can also cause bleeding.
- Continue with all other medications unless otherwise specified.
- Notify your surgeon if you have any abrasions or pimples around the knee.
- Please bring any X-rays, MRI scans or other investigations you have had done which may be relevant to your surgery.
- Bring a list of medications with you to give to the anaesthetist.
You are advised to stop smoking for as long as possible prior to surgery.

Insertion of graft…

Graft in place…
The hamstring tendons are harvested through a small incision just below the knee and are fashioned into a new graft which takes the place of your old cruciate ligament. Tunnels (holes) are then drilled in the tibia and femur (the two bones making up the knee joint) and the graft is passed trough this tunnel. The graft is then fixed with various devices at each end to stabilise it and allow it to heal to the bone. The fixation devices vary and are surgeon specific.
This surgery is mainly done using an arthroscope using small incisions approximately 1cm each. The inside of the knee is thoroughly visualised and any other problems such as meniscal tears or damage to the joint lining (articular) cartilage are treated at the same time.
During surgery local anaesthetic is injected into the knee to reduce the amount of pain you will feel. Pain relieving medication will be provided for you both in hospital and at home.
There may be a drain in your knee which will be removed prior to discharge. You will have a dressing on your wound and a compressive wrap.
Most patients go home the day following surgery but some may go home the same day.
You will be seen by a physiotherapist prior to discharge who will teach you how to use crutches and show you some simple exercises to do at home. Your dressing should be left intact until your first postoperative visit.
Ice packs should be used regularly to reduce swelling.
Your graft is strong enough to put all your weight on your operated leg. You can walk around but rest as much as possible for the first week and elevate your leg when sitting. Most patients require crutches for a week or so.
Pain is variable and prescription pain killers may be required for a week or two.
You may shower but not bath or swim prior to your review. It is normal to have blood under the dressing. If there is excessive ooze the dressings can be changed by someone experienced in wound care. If concerned please contact your surgeon.
You will be followed up in the rooms about 10 days after your operation when the dressings will be removed and the wounds inspected. The surgery and any other findings will be explained to you.
If there is any redness, increased swelling or you have temperatures you should contact the rooms or the hospital where the surgery was performed so they can contact your surgeon.
Time off work depends on your work requirements and is very variable. Office workers usually require 2 weeks off work and manual labourers 2 to 3 months or longer.
Physiotherapy is an integral part of the treatment and is recommended to start as early as possible. Preoperative physiotherapy is helpful to better prepare the knee for surgery. The early aim is to regain range of motion, reduce swelling and achieve full weight bearing.
The remaining rehabilitation will be supervised by a physiotherapist and will involve activities such as exercise bike riding, swimming, proprioceptive exercises and muscle strengthening. Cycling can begin at 4 weeks, jogging can generally begin at around 3 months. The graft is strong enough to allow sport at around 6 months however other factors come into play such as confidence, fitness and adequate fitness and training.
Professional sportsmen often return at 6 months but recreational athletes may take 10 -12 months depending on motivation and time put into rehabilitation.
The rehabilitation and overall success of the procedure can be affected by associated injuries to the knee such as damage to meniscus, articular cartilage or other ligaments.
Complications
Despite advances in surgical technique and the utmost care being taken during surgery, complications can still occur. It is very important for patients undergoing this operation to understand the reasons for the procedure and to have a major role in making an informed choice to proceed with surgery rather than non surgical treatment.
Conclusion
In general this procedure is very successful but complications can occur with any surgical procedure. Other rare or unexpected complications can occur. This is an elective procedure and as the patient you need to make an informed decision on whether or not to proceed with surgery.
