Inside This section
Cartilage Transfer
What Are Cartilage Lesions?
Articular or hyaline cartilage is the specialised tissue lining joints allowing smooth pain free motion of a joint. A lot of people refer to the meniscus as cartilage but this is incorrect. Articular cartilage is normally extremely smooth and is able to absorb shock and the extreme loads placed upon it. When damaged it is not able to repair itself. When the damage is severe it results in pain, catching, swelling and eventually arthritis.
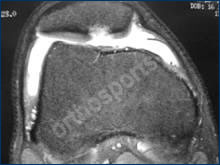
MRI Scan

Cartilage Lesion behind knee cap
There are continual advances in techniques to repair localised injuries to articulajoinr cartilage before arthritis occurs. One such advance is a chondrocyte or cartilage transfer procedure. This process has been developing over the last ten years and is currently a viable alternative for certain patients with cartilage lesions.

Cultured cartilage is cut to size

Glue is used to fix new cartilage cells
Who is suitable for a Chondrocyte Transfer Procedure?
- Pain well localised to a specific part of the knee.
- Young patients 15-50 years.
- Well localised lesion, i.e. lesions in one area rather than all over the knee.
- No instability of the joint (i.e. no significant ligament damage).
- Normal limb alignment-not too knock kneed or bow legged.
- Well motivated for rehabilitation as lots of physiotherapy required (approx 3 months).
- No inflammatory arthritis, i.e. rheumatoid arthritis, gout.
- Body weight less than 1.5 times ideal body weight.

Defect covered with cartilage cells
Articular Cartilage Restoration
What Is Done?
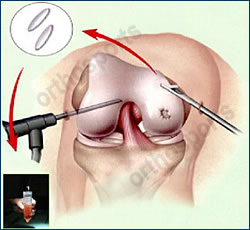
Cartilage cells harvested with arthroscope
A piece of normal cartilage is taken from your knee at the time of arthroscopy from an area it is not needed. This is then sent to a laboratory where it is cultured (i.e. the cartilage cells are grown) and stored for later use. At a second operation;6 weeks to 6 months later; the knee joint is opened up, the lesion is debrided to make a smooth defect and the cells which are on a special membrane much like a piece of felt are placed into the defect.
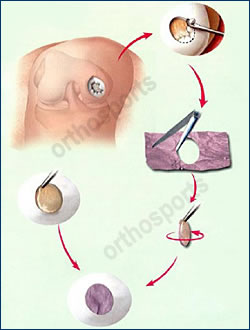
Patch cut to shape and placed into defect
Post-Op
This procedure requires prolonged and well coordinated physiotherapy.
Hospitalisation varies from 2-5 days depending on the size and position of the lesion.
You will usually be none or partial weight bearing for 6 weeks and then increase to full weight bearing by 12 weeks.
The cartilage takes 6-12 months to mature fully and it can be this long before the full benefits of the procedure are realised and you can return to normal activities.
You will require a knee brace to limit the degree of flexion post operatively. A graduated exercise programme will be instituted but will vary from patient to patient. A guide for postoperative care is listed below.
When Can I Return To Sport?
Return to sporting activities and work also is variable and needs to be coordinated with your surgeon and physiotherapist. As a general rule it is not advisable to return to sports involving running and twisting for 12 months.
When Can I Return To Work?
This is a difficult question as it depends exactly what you do at work. If someone drives you and your job involves predominantly sitting then you could go back at two weeks. Physical jobs particularly those involving lifting may take 6 months or longer.
Complications
Any surgical procedure has a risk of complications. These are rare with this procedure, however they can occur. Every precaution is taken to minimise the risk. Complications can be related to the anaesthetic, general in nature it can happen with any surgery or be specific to this procedure.
Excessive swelling and bruising of the leg
This is due to bleeding in the joint and surrounding tissues. It can cause short term pain and make it difficult to bend the knee. To avoid this, ice the leg and elevate it as much as possible for the first week or so. In this procedure a drain is not used as it may damage the graft.
Bleeding
Small amounts of bleeding in the joint are normal. Large amounts of bleeding can occur but are more common in patients with bleeding disorders or those taking antiinflammatory medications. These should be ceased 2 weeks prior to surgery. Excessive bleeding can require aspiration of the knee or occasionally a repeat arthroscopy.
Infection
The procedure is done using antibiotic prophylaxis and in a sterile operating environment to reduce the risk of infection, but it still can occur. Treatment involves either oral or intravenous antibiotics and may involve further operations to wash out the joint. Occasionally this can lead to joint stiffness, destruction of the normal cartilage within the joint or failure of the graft.
Ongoing Pain
This can be unpredictable but is more common in knees with more severe initial damage. If pain does continue then another arthroscopy may be recommended. This procedure if performed is usually to shave part of the graft which may be sitting too proud or has partially lifted off.
Joint Stiffness
Joint stiffness can result from scar tissue within the joint resulting in loss of motion. Treatment consists of physiotherapy or occasionally further surgical procedures. Full range of motion can not always be guaranteed.
Damage to Nerves or Vessels
There are small nerves under the skin which cannot be avoided and cutting them can lead to areas of numbness in the skin below or around the knee. This numbness generally reduces in size with time and doesn’t cause any functional disability. You can get also get areas of hypersensitivity or tingling around the scars. This usually settles with time.
Anterior Knee Pain
Some patients develop pain around the kneecap. This is a result of muscle wasting and inactivity following surgery and usually resolves over time with appropriate physiotherapy and a conscientious exercise programme continued at home.
Reflex Sympathetic Dystrophy
This is a rare condition, the mechanism of which is not fully understood. It involves an overactivity of the nerves in the leg causing unexplained and excessive pain which can go on for many months and may never settle fully.
Deep Venous Thrombosis
This condition is caused by clots in the leg which may require medical management in the form of injections or tablets to thin the blood. Very rarely these can travel to the lungs (pulmonary embolus) causing respiratory difficulties or even be life threatening.
Allergic Reactions
Allergic reactions to medications or materials used in the operating room.
Wound Breakdown
This occurs when small areas of the wound may not heal and may need to e resutured. This can sometimes result from reaction to the sutures just under the skin.
Instrument Breakage
Unsightly or Thickened Scar
Pressure
Pressure on areas of the body in the operating theatre causing nerve damage.
Diathermy Burns
Burns from cautery device used in most open operations (very rare).
Limp
Limp can occur from muscle weakness.
Any medical complication you have heard about can occur especially if you already have a pre-existing medical problem. Such complications include heart attack, stroke, kidney failure, pneumonia, bowel obstruction, bladder infection or obstruction etc. Serious medical problems can lead to ongoing health concerns, prolonged hospitalisation or rarely death.
Rehabilitation varies greatly between patients as it depends on the size and site of the lesion. No two knees are exactly the same. The weight bearing and degree of flexion depends in particular on the location of the lesion. If the lesion is non weight bearing then the whole process can be accelerated.
Week 1
- Allow wound healing
- Weight bearing – nil
- Motion – nil or slight flexion except if on CPM machine
- Brace – locked as appropriate
- Ambulation – crutches
- Physio – rest
Week 2-6
- Weight bearing – none to partial
- Motion – passive up to 90 degrees
- Brace – limited flexion
- Ambulation – crutches usually non weight bearing
- Physio – reduce swelling, closed chain, isometric quads, gentle cycling, walking or treading water in a pool
Week 6-12
- Weight bearing – progress to full
- Motion – progress to full
- Brace – discard
- Ambulation – wean off crutches
- Physio – open chain, proprioceptive exercises, resisted cycling, swimming avoiding breaststroke
Week 12 -52
- Gradual increase in all exercises to strengthen quads and hamstring muscles, jogging at 6 months, sport by 12 months
Summary
This procedure has good results for localised articular cartilage lesions. Without treatment a lot of these lesions progress to arthritis. It does involve quite a lot of rehabilitation and commitment to physiotherapy but once this is over the majority of patients are happy with their outcome.
