Inside This section
Knee Arthritis
Introduction
The knee is the largest joint in the body and is the joint most commonly affected by osteoarthritis. There are many factors that contribute to the development of osteoarthritis. These include injury, obesity, overuse, poor alignment, certain sporting activities and family history.
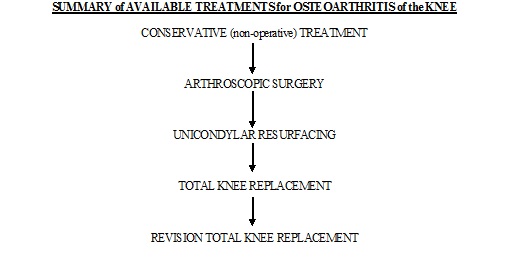
Treatment for osteoarthritis of the knee depends on the stage and severity of the condition and the age and physical requirements of the patient. In general, the initial treatment for early osteoarthritis is non surgical. As the condition progresses (which it invariably does) surgical treatment may be required. This ranges from minor procedures such as arthroscopy to major operations involving total joint replacement. The treatment that is recommend to help manage the painful, arthritic knee has been carefully chosen based on the patient’s symptoms, needs and requirements. As the response to the treatment is noted the treatment required may change to take this into account.

Normal Knee

Osteo-arthritis of the medial or inside compartment of the knee

Bowing of the legs
To view the animation of Knee Arthritis please see the video below
Osteoarthritis of the Knee
Viscosupplementation for Arthritis of the Knee
Treatments for the arthritic knee include the following:
Conservative (No surgery) Treatments
This is always a good place to start and if in the early stages of arthritis can give good results for long periods of time. Successful conservative treatment can delay the need for surgery for months or years.
Building up your thigh muscles allows the shock to pass through the muscle rather than through the inflamed joint and relieves your pain. You can achieve this by doing regular quadriceps (thigh muscle) strengthening exercises. Leg raising or leg extension exercises using ankle weights to strengthen the quadriceps muscle group can help support the knee joint during load and lead to better function and reduce symptoms. 240 repetitions per leg per day (8 sets of 10, three times per day) are required.
Have a course of physiotherapy. A good physiotherapist can help with strengthening exercises and other physical techniques to help maximise knee function and mobility.
Take up a low impact exercise programme. Swimming, walking and stationary cycling are excellent ways to keep mobile and retain function of the knees. Joint surface cartilage is nourished by synovial fluid which requires movement for optimal penetration to the cartilage cells in the deeper layers. Movement is vital for joint function.
Reduce weight if required. More than half of Australian adults are overweight and excess weight places enormous stress on the knees and leads to early arthritis. A GP will give advice on dieting, exercise, and possibly medication. It may be helpful to seek advice from a dietician. Approximately three times your body weight goes through each knee with each step you take. Sensible weight reduction will definitely reduce the pain of osteoarthritis.
Try a course of cartilage supplements. There is very little science behind the use of supplements for arthritis. Some people find that they work very well and some people find that they do not work at all. If trying a supplement I suggest using it for a month and then stop it. Once stopped look for a worsening or deterioration in symptoms. If symptoms are the same on and off the supplement then it is almost certainly not helping. If symptoms become worse after stopping then start the supplement again. I am not aware of any evidence that any supplement can actually reverse the arthritic process or be helpful as a preventative agent. There are many reports of patients benefiting from taking these compounds and the chance of suffering side-effects appears to be very small. The exact mechanism of action of these compounds remains unknown.
Anti-inflammatory medications are very useful in treating the symptoms of arthritis although they do not appear to affect the underlying condition. It is reasonable to take anti-inflammatories as long as complications and side effects do not occur. Common side effects of non-steroidal anti-inflammatory drugs (NSAID’s) include dyspepsia, reflux oesophagitis, stomach and duodenal ulcers, fluid retention, hypertension, and asthma in susceptible individuals (heartburn, reflux and kidney problems). Some patients tolerate NSAID’s for years without suffering complications.
Cox 2 inhibitors are a relatively new class of NSAID that gives relief of pain and symptoms of arthritis but has fewer of the side effects of traditional NSAID’s.
Treatments delivered by injection
Cortisone injections into the arthritic knee may reduce inflammation and relieve symptoms for a while but do not affect the underlying disorder. The injections do not cause skin problems or thinning of the bones like cortisone tablets and can give good pain relief for a period of time.
Visco-supplementation (‘tricking’ the body into thinking it has normal joint lining fluid again) with hyaluronic acid based fluid substitutes may give relief of symptoms of arthritis for several months and may put off the need for surgery in some patients.
Surgery
As the arthritis in your knee progresses the non surgical treatments become less effective in relieving symptoms. In such instances surgical treatments may be required.
Surgical options range from minor operations conducted on an outpatient basis to major procedures such as total knee replacement. The main surgical procedures used to treat osteoarthritis of the knee are:
Arthroscopy (keyhole surgery – no overnight stay required)
Arthroscopy involves inspection of the inside of the knee joint with a small telescope and camera. The image is projected onto a television monitor via a fibre optic cable and allows me to fully inspect all of the interior structures of the knee joint without needing open surgery. Despite the fact that the incisions are quite small, a large amount of surgery can be performed within the knee. Arthroscopic surgery is usually performed on a ‘day only’ basis (an outpatient procedure). The aim of this procedure in the arthritic knee is to examine the specific location and severity of the arthritis. I then remove loose bodies and floating cartilage, treat meniscal tears, remove excess and inflamed synovium and wash out debris from the knee.
Satisfactory results are achieved in about 60% of patients. The results of arthroscopy in the arthritic knee are difficult to predict pre-operatively and can be disappointing. It is possible for symptoms to increase following arthroscopy for a few months and if a satisfactory result is not achieved further surgery may be required.
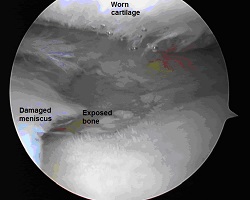
Arthroscopic view of an arthritic knee.
The joint surfaces are rough and the meniscus is torn.
Unicondylar Knee Resurfacing (Partial Knee Replacement)
This operation is suitable for patients who have moderately severe arthritis affecting one side of the knee joint. The procedure involves removal of some bone and replacement of the damaged joint surfaces with metal and plastic implants. The operation is more conservative than total knee replacement, has a shorter hospital stay and faster recovery. The implant may not last as long as a total knee replacement and may need to be changed to a full knee replacement after 8 to10 years.
Patients who have had this operation usually report excellent function and a more natural feeling knee than those with a total knee replacement.
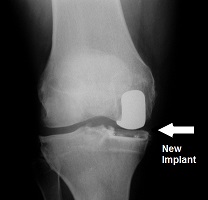

Partial or unicondylar replacements preserve the intact joint surfaces and only replace the damaged area.
High Tibial Osteotomy
Osteotomy literally means cutting of bone. During an osteotomy the bone is cut and its position is changed in order to shift the pressures from one part of a joint to another. The idea is that the bone is cut and realigned to take pressure off the affected part and put onto a better part of the joint.
INDICATIONS
- Patients are generally young (under 55 years of age) and active
- They have arthritis affecting one part of the joint
- They have a good range of motion of the joint
- They have good bone quality
- They are able to non weight bear on crutches
- They are committed to rehabilitation
CONTRAINDICATIONS
- Inflammatory arthritis
- Infection
- More than one compartment involved
- Stiffness
- Obesity
- Over 65 years of age

Opening wedge osteotomy

Closing wedge osteotomy
For more information on Osteotomy please click here
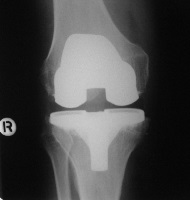
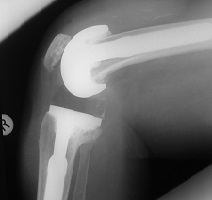
Total Knee Replacement
As the arthritis progresses and the entire joint becomes involved it may be necessary to consider a total knee replacement. This operation involves removal of about 1cm of bone from the end of the thigh bone (femur) and a similar amount from the top of the shin bone (tibia) to allow insertion of the metal and plastic components. This procedure is a major operation and requires about a week in hospital and about 2 weeks in a specialist rehabilitation facility. The physiotherapy in the first month is very demanding and it can take 6 months to be totally satisfied with knee function (Satisfactory results are seen in 90-95% of cases). Unfortunately the plastic can wear out so your knee replacement may not last a lifetime. Some people need a second operation 10 or 15 years after their first one but there are many reports in the literature of 15 years or more satisfactory function following total knee replacement.
Total knee replacements can be inserted with or without bone cement.
Cemented total knee replacement

Cementless total knee replacement
In a total knee replacement all of the damaged joint surfaces are replaced with the metal and polyethylene prosthetic components.
For more information on Total Knee Replacement please click here
Revision Total Knee Replacement
If a knee replacement wears out a revision replacement will be required. The operation involves removing the old implants and replacement with a new knee and may require bone grafting or other specialised techniques to achieve a satisfactory result. This is a major surgical undertaking but with careful planning a successful result can be anticipated in over 90% of cases.

Revision knee replacements involve larger implants and require more bone removal.