Inside This section
Knee Replacement
What Is A Knee Replacement?
Total knee replacement began in the 1970’s. Since then it has become a very common procedure. The aim of the operation is to replace the bottom end of the femur and the top end of the tibia with a man made device (prosthesis). The back surface of the patella is also commonly replaced. These devices are combinations of metal and plastic and occasionally ceramic materials. They are fixed to the bone either using bone cement or by using prosthesis with a rough surface, which relies on your bone growing on to the implant for long term stability. It may be reinforced with screws on the tibial side. In between the two components is a special plastic liner made out of polyethylene.
Knee Anatomy
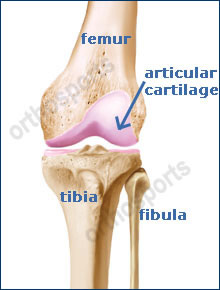
Normal Knee Joint
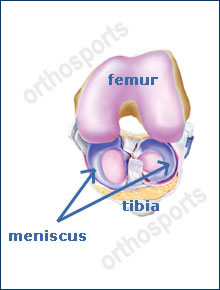
Normal Knee Joint (view from above)
The knee joint consists of the femur, tibia and patella. The femur or thighbone is the bone connecting the hip to the knee. The tibia or shinbone connects the knee to the ankle. The patella or kneecap is the small bone in front of the knee. The fibula is a shorter and thinner bone running parallel to the tibia on its outside. The joint acts like a hinge but with some rotation.
The knee is connected by strong ligaments and surrounded by muscles. The ligaments of the knee joint stabilise the knee allowing it to function normally. The cruciate ligaments (anterior and posterior) are important structures, which guide the knee in its normal motion.
Articular cartilage is the smooth surfaces at the end of the femur and tibia. It is the damage to this surface, which causes arthritis.
The meniscus is a specialised structure within the knee joint between the femur and tibia. There is a medial and lateral meniscus. These help distribute load, absorb shock, and stabilise the knee and aid in lubrication.
Knee Replacement
What Causes A Painful Knee?
When one or more parts of the knee are damaged it can become painful and movement becomes restricted. Over time cartilage (the smooth covering at the ends of the bone in the joint) starts to crack or wear away. When this happens the bones making up the joint, rub together.
No matter what age you are, a knee problem may keep you from activities you enjoy. Pain and stiffness may even limit your day-to-day activities. Problems with the knee joint tend to build up over time.
Any of the problems below may lead to joint damage and hence knee pain…
Osteoarthritis
As time goes by, normal wear and tear can add up. Cartilage may begin to wear away (osteoarthritis). As the bones rub together they become rough and pitted. Previous menisectomies and damage to the anterior cruciate ligament inevitably lead to osteoarthritis.
Inflammatory Arthritis
This is a group of conditions where the lining of the joint becomes inflamed and secretes material that destroys the joint cartilage. In these conditions more than one joint is usually affected. The joints are hot, swollen and painful and deformity is common.
Avascular Necrosis
This can occur for no reason (idiopathic) or can be secondary to a number of conditions such as long-term use of alcohol or steroids. It is due to loss of blood supply to the bone. If the bone dies (necrosis), the joint will become arthritic. This pain often comes on quite suddenly and may increase rapidly. This can happen at any age. There are many other causes of this condition but they are rare.
A bad fall or blow to the knee can break (fracture) the bone. If the broken bone does not heal properly the joint may slowly wear down like a tyre that is not balanced.
Ligament Injury
Injuries to ligaments causing instability of the knee can and usually do lead to premature arthritis.
Childhood Knee Problems
Occasionally knee pain results from a problem, which may have started in childhood such as osteochondritis dissecans, trauma, and juvenile rheumatoid arthritis.
Note – Osgood Schlatters disease does not cause arthritis.
Infection
Infection can destroy the cartilage lining leading to osteoarthritis.
- A bad injury that did not heal properly
- Long term exposure to sports or heavy manual labor
- Other rare diseases affecting bones or soft tissues can also cause severe pain in the knee and may lead to arthritis

X-Ray – Osteoarthritis of knee
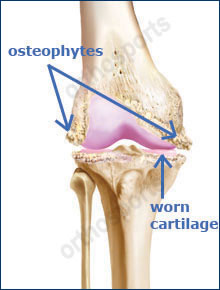
Typical manifestations in arthritic knee
What Are The Benefits Of A Knee Replacement?
You do not have to live with a painful knee for the rest of your life. During this surgery your problem knee joint is replaced with an artificial joint (a prosthesis). After a knee replacement you can look forward to moving more easily and without pain. Most people gain all the following benefits…
- Stops or greatly reduces knee pain.
- Improves quality of life by allowing you to do your activities of daily living and low impact activities in greater comfort.
- Enables you to sleep without pain.
- Provides years of reliable function. Most total knee replacements last for many years.
Indications
When you have arthritis on your X-ray and pain and stiffness from your knee joint cause some or all of the following…
- Severe disability.
- Stops you or makes it difficult to perform your job.
- Interferes with your leisure activities.
- Interferes with your walking or mobility.
- Wakes you at night despite non-operative treatment such as drugs.
- When conservative treatment such as analgesia, anti-inflammatories, weight loss, physiotherapy and aids like crutches or a cane has failed.
Remember, knee replacement is an elective procedure and should only be performed when you are no longer prepared to put up with your pain and disability and understand the benefits versus the risks involved.
Pre-Op Instructions
You will be requested to attend a pre admission clinic. At this clinic, the following will be attended…
- Blood Tests – You will have simple blood tests to make sure your blood count is normal.
- ECG – A Cardiograph of your heart will be taken to make sure you have no underlying cardiac problems.
- X-Rays – Always bring X-Rays of your knee to hospital.
- Urine Sample – a urine sample is required to make sure you do not have a urinary tract infection. An infection anywhere before surgery e.g. infected toenail, skin lesion, throat infection, gum or dental infection can greatly increase your chances of infection of the joint replacement following surgery. If an infection is found it can be treated with simple antibiotics prior to surgery.
- INFORMATION – The clinics are a good opportunity for you to ask any questions you may have of your upcoming surgery.
- Cease aspirin and anti-inflammatory medications (e.g. voltaren, feldene) 10 days prior to surgery as they can cause bleeding.
- Cease any naturopathic or herbal medications 10 days before surgery as these can also cause bleeding.
- Continue with all other medications unless otherwise specified.
- Notify your surgeon if you have any abrasions or pimples around the knee.
- You are advised to stop smoking for as long as possible prior to surgery.
Knee Replacement Procedure
- The anaesthetist will see you before the surgery. They will discuss with you the type of anaesthetic you will have.
- After you are taken to the operating theatre, while you are still awake you are placed on the operating table and set up for surgery with a tourniquet placed around your thigh.
- A urinary catheter will be placed in your bladder to measure your fluid balance during and after surgery.
- A cut is made in the skin and underlying tissues to expose the knee.

Knee with bone cuts
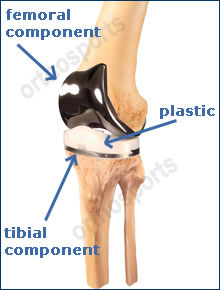
Prosthesis in place
- Special instruments are used to make very accurate cuts in the bone to fit the prosthesis.
- Trial components are put in first to make sure everything fits properly.
- The real components are then inserted.
- Drains are usually inserted.
- The wound is then carefully closed.
- A dressing is applied and you are taken to recovery.
Post –Op
- Your leg will be bandaged from the groin to the toes.
- Your fluid input and output is measured carefully. A drip in the arm will be used to give you fluid, replace blood during the operation and for antibiotics.
- Pain is normal after the operation but if your pain is not reduced be sure to tell the nurse. Pain medication may be injected into a muscle or delivered by IV into the blood stream.
- Patient Controlled Analgesia (PCA) allows you to control your own pain medication. When you push a button pain medication is pumped through an IV line. PCA pumps can provide a steady level of pain relief and with they’re built in safety features you will be assured that you will not get too much medication.
- The drip, drains and catheter are removed on your surgeon’s advice at approximately 24 hours after surgery.
- Blood will be taken 24 to 48 hours after the operation to check your haemoglobin and blood chemicals.
- Your exercise regime will begin as soon as you are capable and this will continue during your stay in hospital and once you are at home. This will be supervised by a physiotherapist.
- You will be discharged approximately 5 days post operatively depending on your progress. In most cases you will be sent to a rehabilitation center before you go home to have hydrotherapy and physiotherapy.
- Sutures are usually dissolvable but if not are removed at about 10 days.
Recovery
- You are in hospital approximately 5 days. At Day 2 you will get up on a frame and then you progress to crutches and then a stick usually by 4- 6 weeks.
- You usually go from hospital to rehabilitation and you are in rehabilitation for one to two weeks. This will include aggressive physiotherapy and hydrotherapy.
- When you leave hospital you will probably still require tablets for pain but no injections. Wean your medications down to panadol as soon as possible.
- It is best to avoid anti-inflammatory if you have arthritis elsewhere for one week to avoid any possible bleeding.
- You lose 60 to 80 percent of your pain by six weeks and 95 percent of your pain by twelve weeks. By twelve weeks you can usually walk as far as you want to.
- Regaining movement early is extremely important, getting the knee straight is as important as bending Do not put anything under the knee even though it feels comfortable as it prevents it from straightening.
- People usually can return to work somewhere from eight to twelve weeks. Heavy manual work may take longer. Normally by three months you can play sports like golf, bowls, stationary bike ride, bush walk, doubles tennis and swim.
Complications
Any operation big or small has risks. The following can occur with any surgery and some rarer complications may also be possible. It is impossible to discuss every complication and there will be some, which no surgeon may anticipate or may never have heard of. The utmost care is taken at all times during surgery to prevent these complications. At Orthosports we are all subspecialised and operate within our defined area of expertise. We believe this minimises the risk of complications.
The following list is not exhaustive and some are explained in more detail in the various sections to which they may be more appropriate.
Surgical Complications
Infection
One of the risks after total knee replacement is infection. Infection may be superficial (i.e. in the skin) or deep (around the prosthesis).The risk is approximately of 1%. If you do get an infection it will be treated aggressively with antibiotics but occasionally re-operation is necessary to clean out the infected material. In very rare circumstances, sometimes the knee replacement is removed and another one put in at a later time, six to eight weeks later when the infection has cleared up.
Fracture (break) of the Femur, Tibia or Patella
This may occur during surgery and may at times not be recognised. It may require more extensive surgery during the operation and very occasionally re-operation a few days later.
Stiffness (lack of movement)
Some people form excessive scar tissue after total knee replacement The average long-term bend of total knee replacement is 110 degrees. If you are not bending past 90 degrees by six weeks you may be readmitted to hospital and under epidural or spinal anaesthetic the knee is forcibly manipulated to break the scar tissue, which is stopping your bend.
Damage to Nerves or Blood Vessels
During the operation, nerves or blood vessels may be damaged. These may be repaired at the time if recognised but may require a second operation to explore or repair any damage. It is very rare that a damaged nerve does not recover on its own. If a damaged nerve does not recover it can lead to poor function of the leg below the joint replacement such as a foot that does not work properly due to weakness or sensory loss.
Blood Clots
Blood clots can form in the calf muscles and they can travel to the lung. These can occasionally be serious and even life threatening. These blood clots will be treated immediately and every measure is taken to avoid these occurring. You will be given a blood thinning agent by injection during your stay in hospital. Stockings will be provided for you which aid in trying to prevent blood pooling in the veins in the calf and you should wear these for six weeks post operatively. A calf pump is also used during the operation on the non operated leg. You will also be given aspirin (unless it is contraindicated in you) to thin the blood after you leave hospital.
The operative scar will always cut some skin nerves so you will have numbness around the wound particularly on the outside (on the side of the little toe). This does not affect the function of your joint but may be irritating to you over the short to medium term. Eventually this numb feeling improves slightly and does not worry most people. Occasionally, instead of a numb sensation you will have burning or a hypersensitive sensation in the wound. This usually settles down over many months but occasionally can be long term and troublesome. Occasionally there is some aching around the scar for many months, which can become worse in cold weather but this usually is nowhere near as uncomfortable as the pain you had before the operation.
Wound breakdown is rare but if it does occur it may require surgery to repair it. You can also get a reaction to the sutures used, causing a stitch abscess, this usually appears as a small pimple on your scar. They can usually be treated with an antiseptic dressing but occasionally require a short course of antibiotics.
Wear
The long-term complication of total knee replacement is wearing of the plastic liner. The joint is like a tyre and if you are hard on the joint, such as someone who does heavy manual labour, plays a pounding sport like jogging or is very overweight; it will wear out faster than a more sedentary person.
Most knee replacements have about an 85 to 95% percent fifteen year survival. There are a large number of factors, which affect the survival rate. Continual improvements in technology make these components more likely to last for a longer period of time. It is our belief that the total knee replacements of today will function better and last longer than those in the past but we won’t know this for another 10 years.
If there is significant wear in the joint then the liner may need to be replaced. Wear can sometimes causes loosening of the joint and the whole joint may then need replacing. This is why we need to follow you up forever. We need to assess your x-ray every few years to make sure that nothing worrying is occurring in the knee joint before you get symptoms. It is extremely important that you do not lose contact with your surgeon during the life of your knee replacement and if you move away from Sydney you should consider talking to your surgeon to recommend a surgeon in another part of Australia.
Osteolysis
This means part of the bone is reabsorbed or disappears. This is a result of small wear particles setting up a reaction in the body causing this bone reabsorbtion. Occasionally we may recommend you have a procedure to change the liner (bearing surface) or bone graft these defects before they become major problems.
Damage to Ligaments
There are ligaments (collaterals, quadriceps, patella) surrounding the knee, which can be damaged before or after surgery. Damage to these ligaments can cause instability of the knee or the inability to straighten the knee. Depending on the circumstances this may require a brace or further surgery.
This means bone forms in the soft tissues surrounding the knee. This can cause discomfort and stiffness and occasionally needs to be excised. This is quite rare in the knee.
Cosmetic Appearance
The knee may be more swollen than the other one or it may be a different shape then prior to surgery. This is normal as we place the knee in its proper alignment during surgery. It looks different because it was an abnormal shape because of the arthritis. Also the scar might be unsightly or thickened.
Breakage of the Implant
This is very rare. If this were to occur reoperation to remove the broken implant and replace it with a new one would be required.
Neuroma Formation
This is an irritation of a superficial nerve resulting in pain, tingling and hypersensitivity around the scar area.
Reflex Sympathetic Dystrophy
This is an unexplained condition where nerves become hyperactive and the limb painful. This may occur following minor trauma or surgery. This usually but not always resolves over time but may require referral to a specialised pain clinic.
Pressure
Pressure on areas of the body in the operating theatre causing nerve damage.
Diathermy Burns
Diathermy burns from cautery device used in most open operations (very rare).
Failure to Relieve Pain
This is not common but unfortunately, some operations may not be entirely successful in relieving pain.
Limp
Limp can occur from muscle weakness.
Bed sores occur from pressure areas on the skin during bed rest.
Other
Any medical complication you have heard about can occur especially if you already have a pre-existing medical problem. Such complications include heart attack, stroke, kidney failure, pneumonia, bowel obstruction, bladder infection or obstruction etc. Serious medical problems can lead to ongoing health concerns, prolonged hospitalisation or rarely death.
Results
This operation is generally very successful. It is an excellent procedure to improve a person’s quality of life. After this operation 95 percent of people are good or excellent. Good means, occasional aches and pains which do not require painkillers and excellent means no significant pain or discomfort. There are some people who will have unexplained pain.
In general, 90 –95% of knee replacements survive 15 years but this depends on a number of variables such as your age and activity level. Again we use the analogy of a tyre. The more you drive on it the quicker it wears out. The better it is looked after and serviced the longer it will last.
Special Precautions To Take
- Remember this is an artificial knee and must be treated with care.
- In general, the more active you are the quicker your knee will wear out.
- You can drive when you have regained muscle control, usually by 6 weeks.
- Avoid situations where you might fall.
- Your knee may go off in a metal detector at the airport. You can receive a note from our rooms to say you have had a joint replacement.
- Prevention of infection is vital. If you have any infections anywhere make sure you see your local doctor straight away for treatment. If you get increasing pain in your joint and are sick and have temperatures you should go to hospital to get checked out.
- USE OF ANTIBIOTICS – Antibiotics should be prescribed if you have an infection anywhere in the body, if you have surgery in contaminated areas such as teeth, nose, bowel or bladder, podiatry treatment or urinary catheterisation.
Activities
- You should avoid pounding activities, which put a lot of stress on the joint.
- Walking is good.
- Swimming in a pool or light surf between the flags is safe.
- Doubles tennis is allowable but anything more aggressive will lead to premature wear of your joint. Contact sports are forbidden and jogging can be detrimental to the long term survival of your joint replacement.
- Skiing on groomed slopes if you are a good skier is acceptable as long as you are aware you can cause significant damage if you fall.
- Bowls and golf should not be a problem.
Conclusion
This operation is one of the most cost effective and beneficial operations done in surgery. By far the majority of people are happy with their joint replacement. Although there is a lot of information above, it is important to read it all so you can make an informed decision to undergo surgery. You must not proceed until you are confident that you understand this procedure and particularly the complications.
Although every effort has been made to explain the complications there will be complications that may not have been specifically mentioned. This is because they are extremely rare. Feel free to access other sources of information from the Internet, other patients and your local doctor. A good knowledge of this operation will take away a lot of the stress you may have.
