Welcome to Question for Physiotherapists June 2021.
This month Dr Paul Annett presents an article on assessing a patient that presents with potentially more than a Sports Injury.
Please feel free to send your questions to education@orthosports.com.au

QUESTION | WHEN SHOULD I BE CONCERNED THAT A PATIENT MAY BE PRESENTING WITH SOMETHING MORE THAN A SPORTS INJURY?
ANSWER | As practitioners in musculoskeletal medicine, we must always be vigilant to the potential medical causes of joint or soft tissue problems. In every patient that presents with a musculoskeletal complaint a consideration of underlying medical issues is paramount. It should be emphasised that just because a patient plays sport and develops a joint or tendon issue, it will not always be due to injury.
Many patients will present initially to a physiotherapist (or other musculoskeletal practitioner) before seeking a medical opinion, so vigilance for unusual conditions is essential.
The type of conditions that should be included include:
- Rheumatoid arthritis
- Seronegative arthropathy (ankylosing spondylitis/psoriatic arthropathy)
- Gout
- Septic arthritis
- Cancer (primary and metastatic)
- Neurological disorders
So what features may alert us that there is something more than meets the eye? A good history is essential. As silly as it sounds an absence of trauma or precipitating event should alert us that there may be an underlying medical issue. In the majority of joint injury, including overuse syndromes, there will be a related initiating causal.
Historically inflammatory symptoms include swelling, morning stiffness (>60mins) and ‘start-up’ pain. Inflammatory conditions typically improve with activity and worsen with rest. They may also be quite sensitive to a trial of anti-inflammatory medications (if no medical contra-indications). Patterns of joint involvement are also important, including spinal and sacroiliac pain in young males with ankylosing spondylitis or small joint involvement of the hands in rheumatoid or psoriatic arthropathy. Consider gout if there is primary 1st MTP inflammation.
Key points may also include a past-history of cancer (the main secondary spread to bone occurs from breast, prostate, kidney, thyroid and melanoma), or a family history of arthropathy. Night and rest pain is also concerning, as are systemic features such as fever and weight loss. Medically conditions such as psoriasis or inflammatory bowel disease (Crohn’s/ulcerative colitis) may be associated with inflammatory arthropathy, as may be a recent viral illness or STD (reactive arthropathy).
Examination findings may include significant swelling from synovitis and soft tissue inflammation of the affected joints, as well as redness, increased temperature, and loss of joint motion. Skin should be assessed for any psoriatic rash, typically occurring on the elbows, knees and in the hair line.
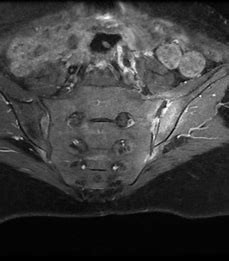
From an investigation point of view any swollen painful joint required an X-ray to assess for degenerative change, osteochondral injury or more sinister pathology (especially in children and past history of cancer). More high-powered imaging such as MRI scanning may help to confirm active joint inflammation, osteochondral injury and early osteoarthritic change. It is especially helpful in the diagnosis of sacroiliitis.
A whole-body bone scan may also be useful to determine a more widespread pattern of joint inflammation in conditions such as rheumatoid and psoriatic arthritis, and also when looking for secondary spread in cancer.
If possible, a joint aspirate should be obtained to assess for inflammatory disorders, crystal arthropathy (such as gout) and to exclude infection.
Blood evaluation is required to detect various inflammatory joint disorders and should include a blood count, kidney and liver function, ESR & CRP (markers of inflammation), rheumatoid factor, uric acid for gout and possibly some other specialised markers such as an ANA (SLE), HLA-B27 (spondyloarthropathy) and iron studies (hemochromatosis).
Management will depend on the condition encountered and diagnosis, but a minimum will include commencing a prescribed medical course of anti-inflammatories for at least 2 weeks. Often trial of a second or even third anti-inflammatory may be required depending on individual sensitivity to the medication.

Ultimately if the level of suspicion is high for inflammatory joint disease then referral to a rheumatologist may be required. Consideration of a more specific disease modifying agent may be required, such as salazopyrine or methotrexate. There are also very exciting recent advances in the use of biologic therapies in the treatment of inflammatory joint disorders.
In summary, underlying medical conditions should be considered in all presentations of musculoskeletal complaints, particularly in the absence of trauma or overuse. A thorough history and examination will help to separate out these cases, and if there is any doubt then referral to an experienced musculoskeletal practitioner can assist in accurate diagnosis.

