Welcome to Question for Physiotherapists November 2025. This month Dr John Negrine discusses syndesmosis injury.
If you registered for the Orthopaedic Updates Webinar 2025 the recorded webinar will be sent by the end of next week. Thank you for your patience.
We wish you all the best for the festive season and thank you for your participation in Orthosports’ Education.
QUESTION | Are we overthinking Syndesmosis Injury?
ANSWER | I pay tribute to my friend and colleague Harvinder Bedi in Melbourne who gave the best talk at the last combined meeting of the Australian and New Zealand Foot and ankle societies on this very subject.

When watching rugby league on the television and the commentator diagnoses a syndesmosis injury it’s time to revisit the so called “high ankle sprain”!
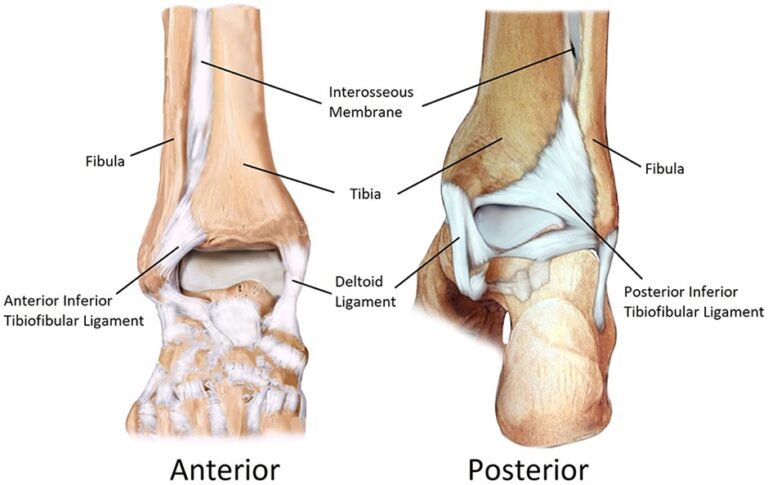
The syndesmosis anatomy is well known to you, the anterior and posterior inferior tibiofibular ligaments as well as the interosseous membrane.
The mechanism of injury typically involves abduction, dorsiflexion and external rotation.
Quick refresher on the grades:
I Partial injury to AITFL, IOM and PITFL intact – considered stable
II Complete injury to AITFL, partial IOM, PITFL intact – may or not be unstable
III Complete injury to AITFL, IOM and PITFL – probably unstable
A good MRI scan with an experienced radiologist will readily diagnose injuries to these ligaments….it will not however diagnose instability and that is (perhaps) the key.
Few would argue that a complete rupture of all three components of the syndesmosis with separation on plain weight bearing films would require stabilisation.
There is however controversy regarding the rupture of the AITFL and interosseous membrane with no demonstrable instability on plain films….the Grade II injury.
James Calder in 2016 (arthroscopy 32:4, 643, 2016) stated that a deltoid ligament tear, frank diastasis on weightbearing films and a positive squeeze test were all good indicators of instability. He correlated this with MRI scans and findings at arthroscopy (3mm of widening was considered unstable.) All his patients were professional athletes.
If stable and managed non-operatively return to sport took 45 days, if unstable and treated surgically 64 days.
Naturally in the professional athlete the fastest return to sport is the key so early arthroscopy is often performed in this country……
Harvinder Bedi postulates (and I agree) that waiting a few weeks in the non professional athlete will do no harm and avoid unnecessary surgery. He also postulates that many grade II and grade III injuries can be managed non-operatively.
What we don’t know is the natural history of what we are seeing on MRI scan. My suspicion is that they don’t all go onto chronic disability and arthritis even in the grade III injuries. Here I am talking about the pure ligamentous injury not the fracture dislocations.


