Welcome to Orthosports Question for Physiotherapists, October 2022. This month Dr Doron Sher discusses imaging for a suspected ACL injury.
Save the Date: Saturday, 12 November, 2022 Annual Orthopaedic Updates @UNSW and via webinar. To register for the live event CLICK HERE. To register for the webinar CLICK HERE
Please send your Questions to: education@orthosports.com.au
QUESTION | MRI REPORTS ARE OFTEN 2 PAGES LONG. WHAT ARE THE KEY FEATURES
YOU LOOK FOR ON AN MRI SCAN OF A PATIENT YOU SUSPECT HAS AN ACL INJURY?
ANSWER | As with all injuries of the knee, a careful clinical examination is required after taking a detailed history. The history and clinical examination will allow you to make an accurate diagnosis over 90% of the time.
Plain Radiographs:
Imaging is then performed to confirm your diagnosis and a standard set of x-rays is obtained.
These are:
- Weight bearing AP (looking at alignment and for arthritis),
- Lateral (looking at patella height and tibial translation)
- Notch view (looking at the flexion portion of the condyles) and
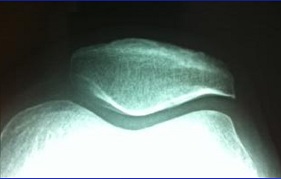
- Skyline view (looking at the patella).



In most instances the plain x-rays will be normal but there are some changes worth looking for:
- A Segond fracture (described by Dr Paul Segond in about 18791) where a fleck of bone is seen adjacent to the tibia. This almost certainly indicates an avulsion near the area of insertion of the anterolateral ligament and in most studies is pathognomonic of an ACL rupture.
- The deep sulcus (terminalis) sign, which is seen as a depression on the lateral femoral condyle at the terminal sulcus. This is the junction between the weight bearing tibial articular surface and the patellar articular surface of the femoral condyle. If you have a bony injury in this area (rather than just a bone bruise) it tends to indicate a higher energy of injury to the knee and the longer-term outcomes tend to be worse when this is present.
- Anterior tibial subluxation relative to the femur (often best seen on MRI) but this is usually a late sign and may indicate failure of an ACL reconstruction or stretching out of the capsule (not usually seen with an acute injury).


If you suspect there may be varus alignment of the limb then 3ft standing xrays are needed because a varus knee will tend to stretch an ACL graft over time and cause it to fail. Some patients have their weight bearing axis medial to the tibial spines or have an alteration in the slope of the tibia (Decreased slope is helpful in the ACL deficient knee). In these situations, the ACL reconstruction might need to be combined with a high tibial osteotomy, with or without a slope correction.
The x-rays will also show arthritic changes or something unexpected like a tumour.


MRI Scanning
Magnetic resonance imaging (MRI) is a scan which uses a magnetic field to take pictures of the inside of the body. It is especially helpful to collect pictures of soft tissue such as organs and muscles that don’t show up on x-rays.
One way to think of an MRI scan is that of a water imaging device. Normal x-rays image calcium, so they are good to see bones but not good for imaging soft tissues.
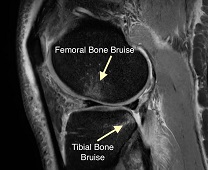
At a simplistic level, the magnet lines up all the water molecules and then lets them go. As they go back to their more natural state they release energy which is read by a sensor and then a mathematical equation (Fourier Transformation) is used to convert this to shades of grey to be seen as images. An example of this is a bone bruise. There should be a very limited amount of water within bone. When the ACL tears and the knee dislocates the 2 bones hit against each other and create damage to the bone with some bleeding internally. This ‘micro-fracture’ of the bone indicates an increased severity of injury.
The investigation of choice is, of course an MRI scan, with most of the pathology being seen on a T2 weighted images. The primary role of the MRI is to confirm the diagnosis or exclude a tear in patients with equivocal physical examination findings. Be aware that not all MRI scans are the same with quality and the reporting of the images varying significantly. That is why it is useful to be able to interpret the images yourself.
The MRI cannot replace careful clinical examination looking for tears of the lateral collateral ligament (LCL), posterior cruciate ligament (PCL), and the menisci. Patients with combined LCL/ACL or PCL/ACL injuries usually need surgery within 3 weeks because an unoperated LCL tear makes early graft failure more likely.
The majority of ACL tears are mid-substance with only 10% being femoral or tibial avulsions. On most MRI scans the tibial ACL insertion will be better visualised than the femoral side so if the rest of the ligament looks normal and the clinical examination does not suggest instability then the ligament is probably not damaged even if the femoral insertion is not perfectly visualised. While inspecting the ACL itself is important there are also secondary signs which correlate well the presence of an ACL injury.
It is ideal to have a sequence that you follow each time when looking at a knee MRI scan.
Sagittal View
Start laterally in the knee and move medially on the T2 weighted images. The first thing we usually see is bone bruising on the femoral condyle (although this may not be present in all injuries and on recurrent instability episodes – about 70% of people with an ACL injury have a bone bruise). This bruising is due to the joint subluxation that happens and is seen (1) in the lateral femoral condyle overlying the anterior horn of the lateral meniscus and (2) on the posterior aspect of the tibial plateau. The femoral condyle bone bruise is seen at the anterior aspect of the lateral femoral condyle between the femoral condyle and the trochlear (where an impaction fracture can take place).
A lateral meniscal tear is seen in up to 85% of patients with an ACL injury but few of these need treatment clinically.
As you move through the notch you will see the ACL first and then the PCL but If the MRI slices are too thick or the axis is not altered to 10-20 degrees of internal rotation the ACL might not be seen on an MRI scan. These days this is rarely the case but this is another reason that clinical correlation with the imaging findings is essential.
Normally, the ACL is a dark structure in the center of the knee. It can be seen starting on the tibia and heading upwards and backwards towards the tibia. It is usually a straight line with no sag (the ‘hammock sign’ showing sagging of the ACL usually means the ligament is functionally deficient even if it seems to be attached to both the tibia and femur).
As we move more medial we start to see fluid in the joint, which is consistent with bleeding from an ACL tear. It is also common for there to be a tear to the posterior horn of the medial meniscus with an ACL injury.
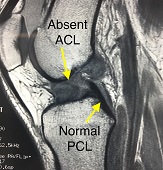
We then move to the coronal images. The normal ACL will be traced from the postero-superior and lateral origin to it’s antero-inferior and medial insertion. As we start to move more posterior we look for bone bruising and we start to see a stump of a torn ACL. Instead of seeing normal contour of the dark ACL substance, we start to see more a balled-up appearance. In this view we can also see the injury to the posterior horn of the medial meniscus.

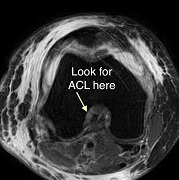
Axial View
Finally, we look at the axial views, although these are not as useful when looking at ACL tears. The ACL is an oval low intensity structure which becomes elliptical in the midsubstance. This is much harder to appreciate if the cuts are not in exactly the right plane. You can see if there is fluid present within the joint and you may be able to see the Segond fracture at the tibia on these images (depending on the slice thickness used).
Re-Injury
In situations where there has been a prior ACL reconstruction then the tibial and femoral tunnels should initially be evaluated on plain xrays. Ideally these are taken with the knee in full extension to accurately calculate
The Tibial Tunnel is best seen on lateral view knee with the knee in full extension. The anterior margin of the tibial tunnel should be behind a line drawn along the roof of the femoral notch (Blumensatt’s line). This ensures that the graft is not impinged on by the bone with the knee in full extension. The center of the graft tunnel should be one-quarter to one-half the distance from the anterior to the posterior tibial cortex but this is more variable that the Blumensaat’s line measurement. In general if the tibial tunnel is too far forward it leads to graft impingement and if it is too far back it leads to ongoing instability.
The Femoral tunnel origin should be posterior to a vertical line drawn along the posterior cortex of the femur. In general, anterior femoral tunnel placement results in excessive tension on the graft in flexion, which restricts ROM, causing tension on the graft fixation site and eventual stretching of the graft.
Posterolateral instability is the most commonly (unrecognized) combined injury and can be seen in 10% to 15% of chronically ACL-deficient knees. The MCL, posterior horn of the medial meniscus, and posterior capsule provide secondary stability in the ACL-deficient knee and must be checked both clinically and on MRI scans because there are no reliable xray signs of this injury.




Summary
This is clearly not an overview to read all parts of the MRI but ACL injuries are common and it is worth knowing some of the common and important imaging signs to look for. In a young active person with these imaging signs early referral for a surgical opinion is appropriate. Not all ACL injuries require surgery but unfortunately many do to return the person to their desired level of sport.
References:
[1] Segond P. Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse. Progres Med 1879
Dr Doron Sher


