Home > Teaching > Injection Techniques > Hand Injections
Hand Injections
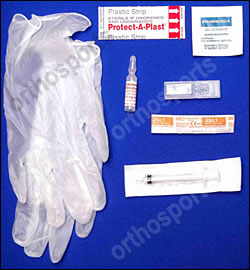
Equipment
- Alcohol swabs
- Gloves
- Bandaid
- Syringe 2.5ml
- use the smallest needle and syringe possible for any given injection.
- it improves your “feel” for the tissues.
- we use – 25 G for base of thumb and carpal tunnel injections.
- 27G needles for trigger finger and De Quervain’s injections.
- Local anaesthetic – 2% Plain Lignocaine – never use Adrenalin.
- Our preferred steroid is Celestone Chronodose.
- it is effective and does not leave a residue in the tissues.
- we don’t use Depot Medrol because of the residual carrier material one notes in the tissues when operating even long after an injection.
- For most hand injections we use 1 ml Celestone + ½ – 1 ml 2% Plain Lignocaine .
Uses
Cortisone injections are useful both for diagnosis and therapeutically .
A good response to a cortisone injection can:
- Help differentiate between Compressive neuropathy, e.g. CTS, and other types of neuropathy, e.g. Diabetic.
- Help differentiate between Carpal tunnel syndrome and Cervical spondylosis and the degree to which each condition contributes to a particular patients symptoms in a double crush syndrome.
- Clarify the source of pain , e.g. STT osteoarthritis and Thumb CMC osteoarthritis. If the examination points strongly to one joint being more painful than another, then inject the most painful joint first . If it is unclear which is the major cause of pain, inject the most distal joint first to avoid confusion from a local anaesthetic block of the surrounding cutaneous nerves.
- Act as a positive prognostic indicator for a good subsequent response to a carpal tunnel decompression.
It is useful for curing up to 50% of trigger fingers and can be used repeatedly over a prolonged period of time to control the pain from osteoarthritis in the hand.
In general, we say to patients that if we inject their base of thumb joint and they achieve pain relief for 6 months, then we will keep injecting them as long as this relief continues. If they only get 1 month relief, then repeated injections are not a satisfactory option.
Contra-Indications…
- Infection of overlying or nearby skin.
- Infected joints (aspirate only).
- Bleeding disorders – we will sometimes inject patients who are taking Warfarin but apply pressure on the injection site for 5 minutes afterwards and get the patient to continue this pressure in the waiting room for another 10 minutes.
- Allergic reaction to similar drug (rare).
Warnings

Overall, the risks of injections performed well are very small. We give patients a Handout Sheet on Cortisone Injections to read while we are drawing up the Cortisone. We then ask them if they have any concerns prior to proceeding…
- Pain when the local anaesthetic wears off – this is more common with joint injections.
- Infection – risk is 1/15000.
- Tendon rupture.
- Elevations of blood sugar in diabetics.
- Cutaneous nerve damage.
- Misplaced injection causing excessive pain.
- Fascial Flushing (up to 40%).
- Post injection flare ( corticosteroid induced crystal synovitis).
- Skin Atrophy.
- Skin hypopigmentation or hyperpigmentation (an issue in De Quervains injections).
- Corticosteroid arthropathy can occur after multiple use (Charcot like joint).
- Osteonecrosis.
- Corticosteroid induced osteoporosis especially if prolonged bed rest or calcium deficient – rarely, transient pituitary inhibition and adrenal suppression.
- Other.
Preparation
Do not draw up the cortisone in front of the patient . This is many patients’ worst nightmare!!


Open the Bandaid prior to injecting so that it can be applied immediately the injection is finished.
Explain the procedure and risks.
Technique
Always lie the patient down – otherwise they may faint during or after the procedure.

Tuck the syringe into your palm so the patient doesn’t see the needle.

Anatomy – identify bony landmarks and mark the line for the injection with your thumb nail.




Clean with alcohol swab then no touch technique.

Ask the patient to squeeze their opposite thumb nail into the pulp of the index finger.

You will need to demonstrate this to them. Make sure they relax the part to be injected.
Say to them that it “should hurt so much with the thumb nail that you won’t feel the injection”.
Most people have a chuckle at this so use this as the time to inject (timing is everything).
Injections should be painless – pass quickly through the skin.
Brace your hand against the patient to steady the needle in case the patient moves during needle insertion.


If injecting a joint insert a small amount of the solution immediately under the skin and wait 20- 30 seconds. This will give the local anaesthetic some time to start working. If you hit bone withdraw slightly and inject a small amount more. You can then move the digit slowly to see if the needle is hitting bone proximal or distal to the joint. eg Basal thumb joint which may be difficult to enter if the patient is not relaxed. Once the peri-articular region is more comfortable the joint can be distracted to allow easier entry into the joint.

Often one feels a “pop” when one enters the joint.
Never inject against resistance.
Remove the needle if patient complains of dysaethesia and re-insert in another line.
Don’t overfill joints with fluid as this can be very painful when the local anaesthetic wears off.
Ask patient to gently move their fingers while injecting.


If the needle moves with finger ROM it is in the tendon!!!
Remove needle quickly and apply local pressure and a bandaid.
Help the patient off the bed and get them to sit down or lie down again if they feel faint.
Encourage patient to rest the affected site – e.g. apply Crepe bandage or a splint if necessary.
After a joint injection inform the patient to “take it easy and have Panadeine when you get home”.
Document the percentage relief of symptoms from the local anaesthetic and ask patient to return in 4 weeks if symptoms persist.
Also ask patient to note what is the best percentage symptom relief once the local anaesthetic has worn off and the injection pain has settled, e.g. percentage pain relief after 1 – 2 weeks?
