QUESTION | I recently had a patient with a partial distal biceps rupture. Why was he offered surgery without trying non-operative management?
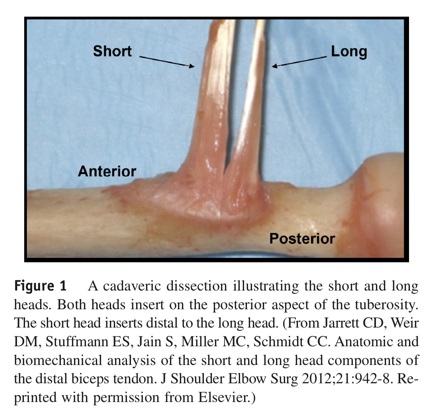
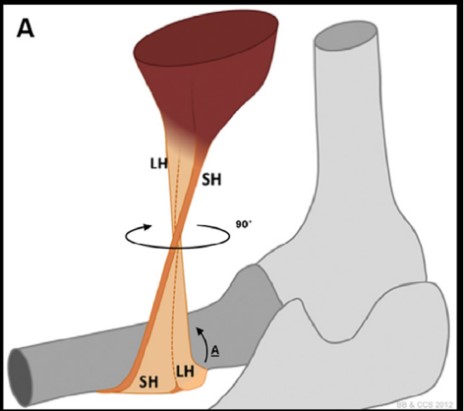
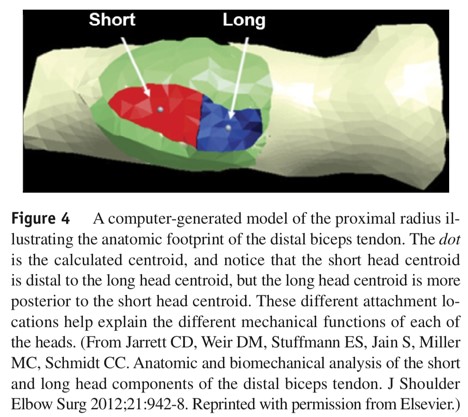
The short head starts medial in the arm but spirals around and inserts more distally on the radial tubercle. It generates 15% more flexion than the long head with the long head being more effective for supination.
Incidence: Distal biceps injuries at the elbow joint account for less than 5% of biceps tendon ruptures overall (the great majority are at the shoulder). They occur at a rate of 2.5 per 100,000 patient-years. Risk factors include smoking as well as increased body mass index. The average age of patients is 47 and more than 90% are male.
Injury Mechanism: Ruptures of the distal tendon near the elbow usually occur when an unexpected force is applied to a bent arm. This is most commonly an activity such as lifting a very heavy object or doing weights at the gym. It can also happen during sports such as a rugby tackle or a snowboarder using the arm to try to break a fall.
Injury Types: The tendon usually tears off the bone but ruptures can occur at the musculotendinous junction (usually with glenohumeral elevation, elbow extension, and forearm supination). It is possible for a patient to tear the short head of biceps only and this is usually incorrectly described or reported as a partial tear of the distal biceps tendon. Unfortunately, it is actually a complete tear of the short head with the long head intact. While the patient seems to recover well initially, they never restore full function to the elbow and most patients will eventually come to surgery with a short head tear.
Functional Outcomes: Without surgical repair, patients who have a complete rupture of the distal biceps will notice loss of strength at the elbow. The strength loss will affect both the ability to flex the elbow and supinate against resistance. Typically, patients get fatiguing and cramping in the muscle belly with repetitive use. Some people find speaking on the telephone difficult due to spasm of the muscle. Most people will find a functionally significant loss of supination and flexion strength, as well as decreased resistance to fatigue.
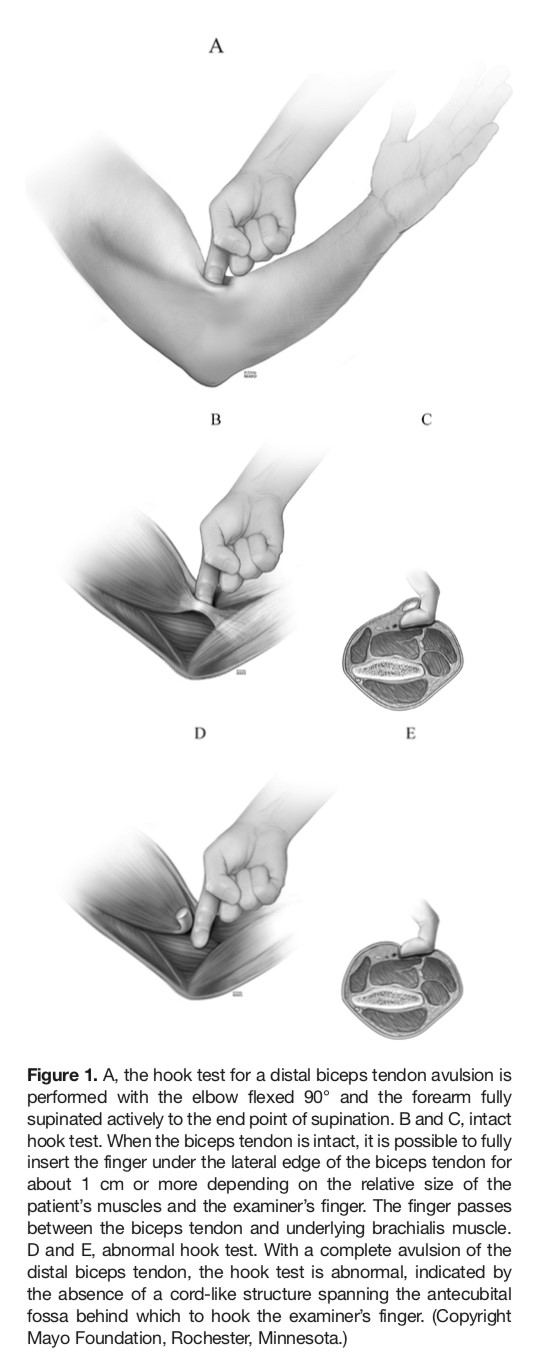
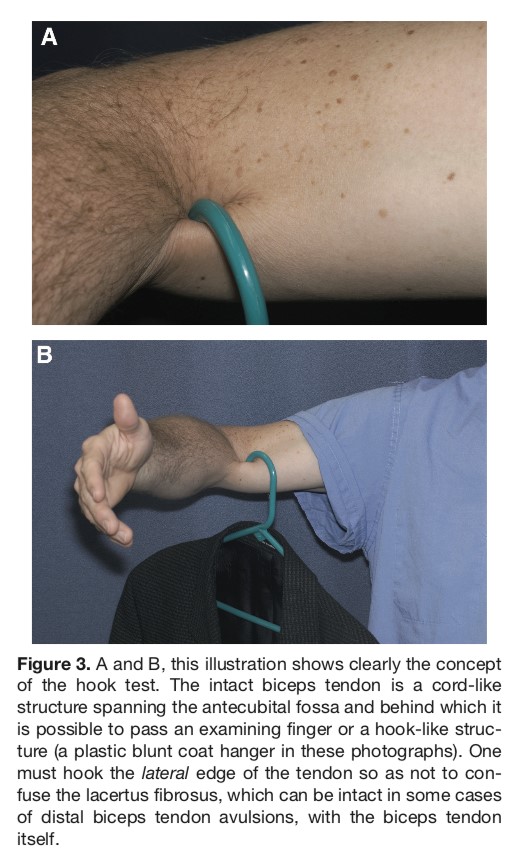
Diagnosis: The patient usually experiences sudden pain over the front of the elbow after a forceful effort against a flexed elbow (eccentric load). There may be a snap or pop and the muscle may curl up into the arm. Swelling and bruising around the elbow are common, usually in the forearm. Movement usually returns over a few days and the abnormal muscle shape becomes more obvious (reverse Popeye sign). The hook test will be positive, which can be both sensitive and specific for complete distal tears. (O’Driscoll SW, Goncalves LB, Dietz P. The hook test for
distal biceps tendon avulsion. Am J Sports Med. 2007;351(11):1865e1869).
Isolated short head tear can be more difficult to diagnose because the muscle does not retract up the arm but does look abnormal. The hook test will also be ‘different’ but not actually positive because the long head is still intact.
Musculotendinous junction tears are rare and often present with antecubital pain, bruising, swelling but a negative hook test.
Imaging: The diagnosis of a distal biceps rupture is made on history and clinical examination. Plain xrays of the elbow should be obtained to ensure that there is nothing unusual with the bone such as a cyst or tumour before drilling a hole in the bone. The only reason to order an MRI is to look for an isolated short head tear. A full tear will be obvious clinically. In my experience the report of a musculotendinous tear is often wrong with the patient having a complete bone avulsion of the tendon most of the time. Ultrasound rarely adds anything to the clinical findings. If an MRI is ordered then a special view with the arm flexed,
abducted and supinated should be performed.
Nonsurgical Treatment:
It has been reported that if the distal biceps is not
repaired most people will lose at least 40% supination strength and up to 30% of flexion strength. In my experience patients also get ongoing cramping of the muscle when holding a phone to their ear or other activities which require prolonged elbow flexion.
If a delayed repair is performed it will allow an improvement of supination and flexion but not normal function. Immediate repair results in normal flexion and supination strength.
Surgical Treatment:
There is no doubt that the best results are achieved with surgery, ideally within 3 weeks and certainly within 6 weeks of the injury. After this time patients are still better off with surgery but a reconstruction procedure with a hamstring tendon may be required rather than a direct repair.
Surgery results in better supination and flexion strength (as well as resistance to fatigue for both motions) and correction of the reverse Popeye deformity.
If the tear is incomplete then surgery may not be needed (or if the patient is elderly or has very low demands of the arm). It is my experience that even patients with a partial tear (usually a complete tear of the short head) continue to be symptomatic and request the surgery eventually.
There are few contraindications to repair.
Surgical Approach:
Single and double incision techniques both work very well. They both have advantages and disadvantages in terms of cosmesis, nerve injury and heterotopic ossification.
The single incision technique is more expensive as
hardware is always required where the two incision technique typically uses bone tunnels only. My preference having tried all the methods is the classic 2 incision technique which does not leave any hardware in the patient and gives excellent results. There is some evidence that the 2 incision technique will allow more normal supination strength restoration.
Postoperative Care: The reattachment site is at greatest risk for failure during the first 1 to 2 weeks after surgery. The arm is placed in a backslab for one week to allow wound healing. The patient then starts an active range of motion programme but limits the use of the arm to simple daily activities for a total of 6 weeks.
If the repair was delayed, a period of time in a hinged elbow brace to allow flexion but prevent extension might be needed. At 6 weeks, gradual strengthening and conditioning can be started for standard repairs. Strengthening is delayed to 10- 12 weeks for high-flexion repairs or allograft reconstructions. Return to heavy lifting is delayed until 3 to 6 months after surgery depending on the quality of the
repair at the time of surgery.
Rerupture can occur after surgery.
Chronic Distal Biceps Rupture: Injuries more than 6 weeks old are more difficult to deal with because they often have tendon shortening, tunnel obliteration or adhesions. The patient may need to be splinted in flexion for a period of time. Despite this full motion is almost always restored by the end of the rehabilitation period. Allograft or autograft reconstructions work very well with some loss of strength and a much longer rehabilitation time.
Summary:
Distal biceps repair can restore near-normal flexion and supination strength. Generally speaking the procedure is a very successful one with patients returning to their previous level of activity.
References:
The Hook Test for Distal Biceps Tendon Avulsion
Shawn W. O’Driscoll, PhD, MD, Lucas B. J. Goncalves, MD, and Patricio Dietz, MD
From the Mayo Clinic, Rochester, Minnesota, Hospital Madre Teresa, Belo Horizonte, Brazil, and
Hospital Base Osorno, Osorno, Chile
The American Journal of Sports Medicine, Vol. 35, No. 11 DOI: 10.1177/0363546507305016
Distal biceps tendon history, updates, and controversies: from the closed American
Shoulder and Elbow Surgeons meeting—2015
Christopher C. Schmidt, MDa, Felix H. Savoie III, MDb, Scott P. Steinmann, MDc, Michael
Hausman, MDd, Ilya Voloshin, MDe, Bernard F. Morrey, MDc, Dean G. Sotereanos, MDa, Emily
H. Bero, BSf, Brandon T. Brown, MMEg
http://dx.doi.org/10.1016/j.jse.2016.05.025

