Welcome to Orthosports Question for Physiotherapists, June 2023. This month Dr Michael Goldberg discusses lateral extra-articular tenodesis and why you would add this procedure to an ACL reconstruction.
Save the Date: Saturday, 4th November, 2023 Annual Orthopaedic Updates. Live event at UNSW and via webinar. More details soon.
Please send your Questions to: education@orthosports.com.au
QUESTION | WHAT IS A LATERAL EXTRA-ARTICULAR TENODESIS AND WHY WOULD YOU ADD THIS PROCEDURE TO AN ACL RECONSTRUCTION?
ANSWER | A lateral extra-articular tenodesis (LEAT) is a procedure that may be used to augment a routine ACL reconstruction, to reduce persistent anterolateral rotatory instability. It is being used increasingly commonly due to high quality evidence that it improves graft survivorship in individuals who are at high risk of graft re-rupture.
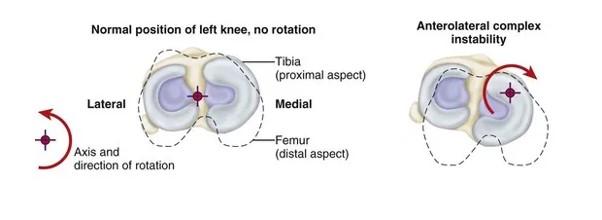
ACL reconstruction does not always completely restore native knee biomechanics, particularly with regard to tibial rotation. This can lead some patients to have persistent knee instability (or a positive pivot shift test) after ACL reconstruction, despite an intact graft. Anterolateral rotatory instability is where the tibia sits relatively internally rotated to the femur (figure 1), due to injury to the normal soft tissue restraints to tibial internal rotation. These include the anterolateral capsule, iliotibial band (including the deep Kaplan fibre attachments to the femur) and the menisci. A LEAT helps to restrain tibial internal rotation, which in turn prevents the pivot shift.
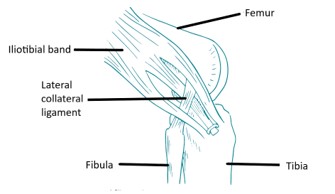
A LEAT is an open procedure which can be added to a routine ACL reconstruction. It adds 10-15 minutes to the surgery. There are multiple techniques for a LEAT, each of which involves re-routing a strip of the iliotibial band under the lateral collateral ligament, to create a restraint to tibial internal rotation. The most common techniques are the Modified LeMaire and Modified Ellison technique. I use the modified Ellison technique, where a 1cm wide strip of ITB is detached off its tibial attachment at Gerdy’s tubercle, passed under the lateral collateral ligament, and then reattached to its original insertion on Gerdy’s tubercle (figure 2).
A recent Canadian, multicentre, randomised controlled trial provides compelling evidence for the effectiveness of LEAT. The Stability study, published in 2020, looked at patients at high risk of graft rupture. It compared patients undergoing ACL reconstruction using hamstring autograft, with an ACL reconstruction plus LEAT. The results showed that the addition of the LEAT reduced the rate of re-rupture from 11% to 4% at 2 years of follow-up.
I therefore consider a LEAT in all patients who are likely to have a high risk of graft rupture. These tend to be patients who are young (< 25yrs), have generalised ligamentous laxity, have a high grade pivot shift on examination, and a desire to return to pivoting or contact sports. I also add a LEAT in all revision procedures.
LEAT often increases post-operative pain and stiffness in the first few months after surgery. LEAT also tends to delay return to sport by approximately 1 month. I do not alter my normal ACL rehabilitation protocol in patients having a LEAT.
Further reading:
Getgood AMJ et al. Lateral Extra-articular Tenodesis Reduces Failure of Hamstring Tendon Autograft Anterior Cruciate Ligament Reconstruction: 2-Year Outcomes From the STABILITY Study Randomized Clinical Trial. Am J Sports Med. 2020 Feb;48(2):285-297.


