This month Dr Doron Sher discusses rehabilition after a Reverse Shoulder Replacement. Please feel free to send your questions to education@orthosports.com.au

QUESTION I I had a patient who was allowed to remove her sling and use her arm the day after a reverse shoulder replacement. We used to keep patients in a sling for 6 weeks before starting their rehabilitation.
ANSWER | What has changed?
Reverse shoulder replacement is usually performed in elderly patients. The operation is typically performed when the patient has severe pain from arthritis with a rotator cuff tear or they are unable to lift their arm to shoulder height. Other indications include an irreparable rotator cuff, arthritis with a poor quality rotator cuff that is likely to fail after a primary shoulder replacement, significant glenoid retroversion, instability or bone loss (even if the rotator cuff is intact). The design of the prosthesis means that the Deltoid, rather than the rotator cuff, moves the arm.
Immobilising these older patients in a sling is a huge imposition as many of them live alone and struggle with activities of daily living, even when using both hands. In the past many patients chose to live with the pain rather than go through the ordeal of wearing a sling for 6 weeks.

The original “Grammont” style prosthesis medialised the humerus a long way to allow the centre of rotation to be shifted to allow the deltoid to take over the function of the rotator cuff. The subscapularis was very important to restore stability to the shoulder with this design and typically physiotherapy was not started until the Subscapularis had started to heal.
Dislocation rates and range of motion were negatively impacted in situations where the subscapularis could not be repaired or did not heal. Six weeks in a sling was necessary to allow the Subscapularis to heal.
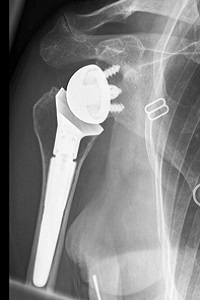
The newer designs of the prosthesis combine medialisation of the glenoid component with lateralisation of the humeral component. Generally the subscapularis is not repaired as part of this procedure as it does not offer additional stability to the construct.
Since we do not need to wait for the subscapularis to heal, the patient can use and move the arm immediately. There are still certain positions, such as loading in internal rotation pushing up out of a chair, which can lead to instability of the prosthesis and should be avoided early in the rehabilitation phases.

- Generally these patients are older and often quite osteopaenic. Since their bones are softer, fixation of the glenoid component in the bone is not always perfect. Early movement places large forces through the glenoid / bone interface which can then displace.
- The other issue related to osteopaenia is the forces placed on the acromion by the pull of the deltoid. Many of these patients have not been able to lift their arm above shoulder height for many years. The new prosthesis allows far better range of motion than what they had previously but this means that the deltoid is now pulling quite strongly on the acromion. The bone in the acromion needs to remodel and become stronger, which takes time. It is possible to develop a stress fracture of the acromion if the loading happens faster than the bone remodelling.
- The day after the operation they are allowed to remove the sling and use the arm to eat, dress and wash their face. If they have pain then the sling is reapplied for short periods of time. As time passes they use the arm for simple activities of daily living and by 7-10 days very few patients are using the sling during the day. It is important to re-apply the sling at night time, both for comfort and to ensure the arm does not move into a potentially unstable position while they are asleep.
- After about one month, once there is adequate bony ingrowth and soft tissue healing, the night time sling can be discontinued. The patient will now commence an active range of motion programme but no strengthening (to allow acromial remodelling).
- If at 2 months the patient does not have adequate range of motion or function they commence a formal physiotherapy programme. There are very few studies comparing early mobilisation with 6 weeks of immobilisation after reverse total shoulder replacement. Most of these studies show no significant difference out to 2 years.
- Since there is no disadvantage in allowing early usage of the arm it makes sense to allow the patient more independence as soon as possible after surgery without compromising implant fixation or creating stress fractures.
The design of the reverse shoulder replacement has changed over time. This has allowed pain relief and faster restoration of function in a patient population where the thought of spending 6 weeks in a sling is daunting and not necessary. For many patients this makes the decision to proceed with surgery easier, knowing that they will have pain relief, restore function and quickly regain their independence.
Dr Doron Sher

