Welcome to Orthosports Question for Physiotherapists September 2024. This month Dr Doron Sher discusses Spontaneous Osteonecrosis.
REMINDER TO REGISTER Orthosports Annual Orthopaedic Updates, Saturday, 9th November 2024, Live event @UNSW Click here to register
Webinar (live and recorded) Click here to register

QUESTION |What is Spontaneous Osteonecrosis?
Spontaneous Osteonecrosis of the Knee (SONK or SPONK)
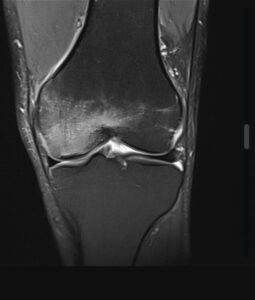
Spontaneous osteonecrosis of the knee is a progressive disease of the subarticular bone that can lead to subchondral collapse. It was first described by Ahlback et al. in 1968 as a medial femoral condyle (MFC) focal lesion and they commented that the early stages of the process are often undetected. Patients with SONK mainly complain of acute onset of pain in the knee and report no previous trauma.
It can be found in nearly 10% of people over 65 years of age and about 3% of people over 50. It is far more common in females.
The most common location is the medial femoral condyle with the medial tibial plateau next most common and it is only rarely seen in the lateral femoral condyle. It is usually found in 1 location only.
Typically patients have pain on weight bearing but not at rest. They often have more tenderness of the bone than the joint margin.
Most patients initially feel pain in the back of their knee and often a pop while they are gardening, kneeling or doing other activities with deep knee flexion. A few weeks later they start to develop medial joint pain, usually from overload of the medial femoral condyle bone and articular cartilage due to the meniscus root being non-functional.
Xrays are often relatively normal but an MRI will show bone marrow oedema and focal subchondral lesions.
What Causes Spontaneous Osteonecrosis?
There are several theories but none of them have been categorically proven to be the cause. The most likely of these is that it results from what were previously unrecognized medial meniscal root tears (posterior horn type 2 medial meniscus root tears). The meniscus root would tear off its attachment in the back of the knee with a simple activity such as squatting or gardening. The meniscus extrudes and fails to act as a shock absorber effectively creating a total meniscectomy in the knee. This leads to a massive increase in bone reaction forces and explains why the condition is almost always on the medial aspect of the knee. This can also happen after a partial meniscectomy with arthroscopic surgery and should always be kept in mind if a patient has an increase in their pain after a knee arthroscopy.
Other theories include:
- Subchondral Insufficiency Fractures: These fractures may lead to fluid accumulation in the bone marrow, causing focal ischemia and subsequent bone necrosis.
- Vascular Injury: This is somewhat speculative
- Osteopenia or Osteoporosis: Individuals with weakened bones are more susceptible to SONK, possibly due to the increased likelihood of insufficiency fractures.
- Idiopathic Factors: In many cases, SONK develops spontaneously without a clear cause, which is why it is termed “spontaneous”.
How to Treat Spontaneous Osteonecrosis
The first step in the treatment is to see if the patient has a meniscal root tear. If they do we then look at their articular cartilage. If the cartilage is in good condition then the best treatment is to repair their meniscal root tear and rehabilitate the knee.
The patient will need to be non-weight bearing on crutches for a few weeks at least which also unloads the bone and allows any insufficiency fracture to heal.
For patients who have significant arthritis already, the use of crutches and possibly a medial compartment unloader brace may allow the bone to heal and buy some time before moving towards a total knee arthroplasty.
Other non-operative treatments include:
- A period of non-weight bearing to prevent further damage and allow healing.
- Medications such as anti-inflammatory drugs and bisphosphonates.
- Strengthening exercises
- A medial compartment unloader brace
- Teriparatide which promotes bone formation and has shown promising results in reducing lesion size and pain early in the disease process. It does have potential side-effects and should only be prescribed by people experienced in its use.
Surgical treatments include:
- Core decompression to relieve pressure and promote blood flow
- High tibial osteotomy to unload the damage area (only in young patients)
- Joint replacement is the final solution when all else has failed and is very successful in treating this condition.
Most cases of spontaneous osteonecrosis of the knee that are caught early enough can be treated.
They are often due to a posterior horn medial meniscus root tear with extrusion and early diagnosis and treatment is recommended to slow down the progression of arthritis in these patients.
Hopefully this will reduce the number of patients who progress and require joint replacement surgery.