Inside This section
Total Shoulder Replacement
To view an animation of Total Shoulder Replacement, click here.
The Shoulder Joint
The shoulder joint is one of the most complex joints in the body. It has a greater range of motion than any other joint and is a ball and socket type joint. It is made up of bone, cartilage, tendons and muscles, all of which are affected to differing degrees by different forms of arthritis.
Arthritis is a degenerative condition where the lining of the joint (the articular cartilage) wears away, leaving a rough and worn joint surface. Chronic (ongoing) shoulder pain and / or loss of movement are the most common reasons for shoulder replacement surgery and are usually age related. Due to similar age related changes, the muscles about the shoulder (the rotator cuff) may tear as well. This reduces the power and movement of the shoulder. Unfortunately this is a progressive disease and it is not reversible. Fortunately for some people the progression take place at a slow rate and many people will not need surgery for their condition.
Early in the disease anti-inflammatory medications, physiotherapy and a reduction of activities may relieve the symptoms of the arthritis. As time goes by the pain and stiffness eventually become unbearable and it is then time to consider a shoulder replacement.
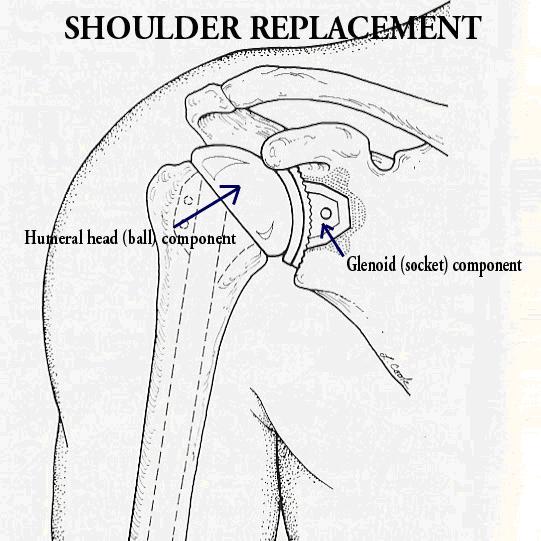
During surgery the damaged parts of the shoulder are removed and replaced with artificial parts (components) called prostheses.
One reason why this type of surgery is not recommended early in the disease process or at a young age is that the artificial shoulder only has a life span of 10 to 15 years. In addition, while the surgery usually works very well, it is not always successful. Although a worn out component can be replaced, the results of a redo (revision) shoulder replacement are not particularly good. Unless there are exceptional circumstances, shoulder replacement is not recommended in patients under 50 years of age.
The prostheses are made of metal and ‘plastic’. The component in the humerus (ball part) is typically made out of a metal alloy of titanium and the component in the glenoid (socket part) of a ‘plastic’ material called polyethylene. These can be ‘cemented’ into place or “press fitted” with screws but the technique will vary depending on the patient’s quality of bone, whether their rotator cuff is intact or torn and whether they have problems with other joints in the body.
Where it is possible, it is best to replace both the ball and socket of the shoulder. Sometimes only the ball part of the joint can be replaced. This is typically when the rotator cuff is torn and not repairable or when the socket is not damaged. This decision is usually made at the time of surgery when the surgeon looks into the joint and assesses the exact amount of shoulder damage.
When the rotator cuff is torn and the bone quality is satisfactory, a “reverse shoulder replacement” is inserted which can make up for the torn rotator cuff.
Pain relief from the surgery is usually very good but not perfect. If your rotator cuff is functioning well you should expect to be able to comfortably get your hand over your head. If the rotator cuff is torn you may only get your hand to touch your head.
Most people have a good range of motion following surgery but few people ever regain a full range of movement.
The operation takes about two hours and a cut is made on the front of the shoulder extending into the upper arm. There will be some permanent numbness around the scar. As indicated earlier, the operation involves cutting out the damaged ball and socket and inserting the artificial components with or without repair of the rotator cuff muscle.
When you wake up you will find your arm in a sling and have a drain coming out of the wound. You will most likely be given enough pain killers to keep you comfortable. The drain will be removed and a waterproof dressing will be placed on the shoulder. You are then able to shower but must leave your arm adjacent to your body even when the sling has been removed. It is very important that you do not lift or rotate the arm at any time. It is important to get out of bed and walk around as soon as you are comfortable. You make very sure the armpit is as dry as possible to reduce the risk of a sweat rash or armpit infection. Ice may be applied to help reduce the swelling and discomfort around the incision and you should inform the nurse if your arm gets too cold or if there are any changes in the sensation of your hand.
On the second day after the surgery you will start an exercise program under the supervision of a physiotherapist. This is for PASSIVE movements only and are performed with the unoperated arm lifting the operated arm over the head, while lying down. This protects the muscles in the operated shoulder from contracting and potentially disrupting the surgical repair. The shoulder takes about six weeks to heal and the exercises are started early to avoid stiffness following the operation.
To increase your comfort during your exercises, you may want to take pain medications 30 minutes before your physiotherapy sessions. The physiotherapist will check your early progress and keep me informed. If possible, a member of your family or a friend should accompany you to the physiotherapy sessions to learn the exercises you should do at home. This person will practice these exercises under the supervision of the physiotherapist first which can then be performed at home.
Approximately four days after the surgery you may be discharged from hospital. The exact timing of the discharge will depend on your pain level, your progress with the exercise program and your home situation.
Once you get home you will need to do exercises four times a day for six weeks. These are passive exercises only and you will not need to see a physiotherapist during this time unless you have difficulty doing the exercises yourself (or do not have someone to assist you with the exercises). The sling must remain on 24 hours a day. It should not be removed for sleeping but may be removed very briefly for a shower, at which time the arm should be kept adjacent to the body. You must not elevate or rotate the operated arm at any time for any reason.
Since the Roads and Traffic Authority does not permit driving a vehicle while you are wearing a sling it is recommended that you not drive for at least six weeks. You will be seen approximately two weeks after the surgery for your stitches to be removed and your movements checked. If the movements are a little slow you will see a physiotherapist but if you are making satisfactory progress your physiotherapy will not start for six weeks. It is important to do your exercises at least four times a day, every day.
You may use your hand for gentle activities directly in front of you and may bend the elbow, wrist and hand but must never move the shoulder. It is best to avoid lying or turning onto the affected shoulder.
You should apply ice to your shoulder before and after exercises to reduce pain and swelling and must not use a heating pad as this will increase swelling around the joint.
At six weeks post operatively your sling will mostly likely be removed and formal active physiotherapy will be started. At this point you will be allowed to lift your arm up under your own power and you will be given a set of exercises using a rubber band. Despite the fact that you will only be supervised by a physiotherapist two to three times a week you must do your exercises at home at least four times a day, every day. It is not unusual to have an increase in pain when you commence active exercise programs.
At six weeks you will be able to lift objects weighing less than two kilograms. You can move your arm in any direction you desire and your exercises and lifting limits will be upgraded from time to time.This will depend on your clinical progress.
It takes approximately six to twelve months for the shoulder to reach its full potential and the exercises are required for that period of time.
Even with an excellent result, you will never have a perfect shoulder. Pain relief is very good but range of motion never returns to normal. This is particularly true if the rotator cuff is torn. By avoiding heavy or repetitive work you make it less likely that the implants will loosen within your shoulder. Racquet sports should be avoided but golf and bowls are allowed. Freestyle swimming should be avoided but for most people breast stroke is OK.
- Fever above 38 degrees Celsius.
- Increased pain unrelieved with pain medications.
- Sudden, severe shoulder pain.
- Increased redness around the incision.
- Increased swelling at the incision.
- A bulge that can be felt at the shoulder.
- Shoulder pain, tenderness or swelling.
- Numbness or tingling in the arm.
- Change in arm length.
- Change in colour and temperature of the arm.
- Change in motion ability.
- Drainage or odour from the incision.
- Any sign of any infection anywhere in your body should be reported to your GP as soon as possible and most likely you will need to start antibiotics.
You will be seen each year following your surgery with an x-ray of your joint. This ensures that the artificial joint is not loosening and that your progress has been maintained. If there is significant loosening or wear of the components, a redo of the replacement may be required. The second time an operation is done has a lower success rate than the initial replacement.
Approximately 80 to 90 percent of patients achieve an excellent or good result.
All operations have potential complications, however, complications are not common with this procedure. This is an operation that can leave you permanently worse off if you do develop a complication. The common ones include but are not limited to infections, nerve and blood vessel damage, dislocations and bone fractures.
The orthopaedic literature documents a 5 percent chance of making you permanently worse off and while it is exceedingly uncommon, there is a very remote chance of you losing complete use of you whole arm. Medical complications can also occur and elderly people with heart disease or diabetes are particularly at risk.
