Inside This section
Cortisone Injections around the Shoulder
Cortisone injections make up a very important part of the treatment of shoulder injuries. In combination with an active rehabilitation program they may significantly reduced the need for surgery in shoulder impingement syndrome.
Cortisone is a potent anti-inflammatory medication. It was only discovered as recently as 1950 (earning a Nobel Prize for medicine for Hench and his co-workers), and has been available in an injectable form since 1951. It acts on both acute and chronic phases of inflammation to reduce both tissue swelling and subsequent scar formation.
Cortisone injections are useful in the treatment of various musculoskeletal conditions, particularly those of acute inflammation (such as acute bursitis), and degenerative joint and tendon conditions.
In the shoulder they are particularly useful in the management of:
- Rotator cuff disease (degenerative tendonosis, impingement, partial tears and subacromial bursitis)
- Adhesive capsulitis (or ‘frozen shoulder’)
- Glenohumeral osteoarthritis
- Acromioclavicular joint disease (osteoarthritis or osteolysis)
Cortisone injections should only be performed in the setting of an appropriate diagnosis based on taking an accurate history, performing a clinical examination and commonly performing investigations. These should include an x-ray as mandatory and may also include an ultrasound or an MRI scan, depending on the indications. They will generally be used after failure of a 4-6 week trial of relative rest, anti-inflammatory modalities and medications and an exercise based physiotherapy program.
Common Misconceptions & FAQ’s
Cortisone injections are painful: The majority of patients expect the injection to be very painful, an most are pleasantly surprised that it isn’t the case. At the time of injection it should hurt no more than a common immunization needle. Around 1:20 patients may have pain that is worse after the injection. This generally occurs for no more than 2-3 days and is related to irritation of the tissue injected from the cortisone itself. This ‘injection flare’ is much less common now as the modern cortisone injections are more water soluble. It is best treated with local ice packs and simple analgesics.
You should only have 3 injections: There is no scientific evidence to support this statement, but it seems to have been set in concrete somewhere along the line. Common sense would suggest if 3 injections given at 4-6 week intervals have been unhelpful then further injections are less likely to be beneficial, but having one further injection if progress is being made is not inappropriate, or indeed dangerous.
Cortisone injections will make me fat and give me weak bones: Taking oral cortisone (or prednisone) for long periods of time can certainly have side-effects, which do limit the use of this very effective drug. These would include weight gain, osteoporosis, diabetes and high blood pressure. A small amount of cortisone is absorbed after an injection, but quickly cleared within 2-3 days. There are no long term side-effects from repeat local injections of cortisone.
Isn’t this injection just a painkiller?: The cortisone injection is not just an analgesic or pain-killer. It works by reducing inflammation, and thus pain secondarily. As such it is treating the pathology, not just the pain. It is important that the injection is followed up with appropriate rehabilitation (see below).
Side Effects
Local cortisone injections may cause some side-effects.
These would include:
- Systemic absorption. Care should be taken in diabetics as blood sugar levels may rise
- Infection – The medical literature suggests this occurs in less than 1:20,000 cases. It can be avoided by using a sterile ‘no touch’ technique with the needle and an alcohol swab
- Crystal flare – As previously mentioned occurs in 1:20 patients and can be treated with ice and paracetamol
- Skin changes – Skin atrophy & pigment loss may occur around the injection site. This is generally a minor cosmetic problem and occurs in less than 1:100 patients
- Bleeding (especially if patient has a bleeding tendency)
- Neuritis – The cortisone may cause minor irritation to nerves if injected around them
Failure Of Cortisone Injections
Cortisone injections make up an important part of treatment of various shoulder conditions. They are, however, not the only method of treatment, but part of an overall management program. The cortisone injections do not cure the condition, but provide a window of symptom relief via inflammation reduction. This then allows pain free rehabilitation exercises to be performed, improving joint motion and muscle strength and function, which ultimately prevent the condition from recurring later on. All cortisone injections should ideally be followed up with a physiotherapy program including manual therapy and an exercise prescription.
Failure of cortisone injections may occur for various reasons. The most important factor to consider is appropriate diagnosis. A rotator cuff injection will not help an acromioclavicular joint problem. This is best addressed by careful taking a careful history and examination, as well as supporting the diagnosis with tests. Correct placement of the needle is also essential. In some cases an imaging support (such as an x-ray) may be used to confirm the needle position. Inadequate follow-up rehabilitation and activity modification is another common reason for failure or limited success of cortisone injections. Sometimes athletes are lazy with their rehabilitation or just don’t want to rest!

Fig. 1. Injection into the sub-acromial space (for rotator cuff disease)
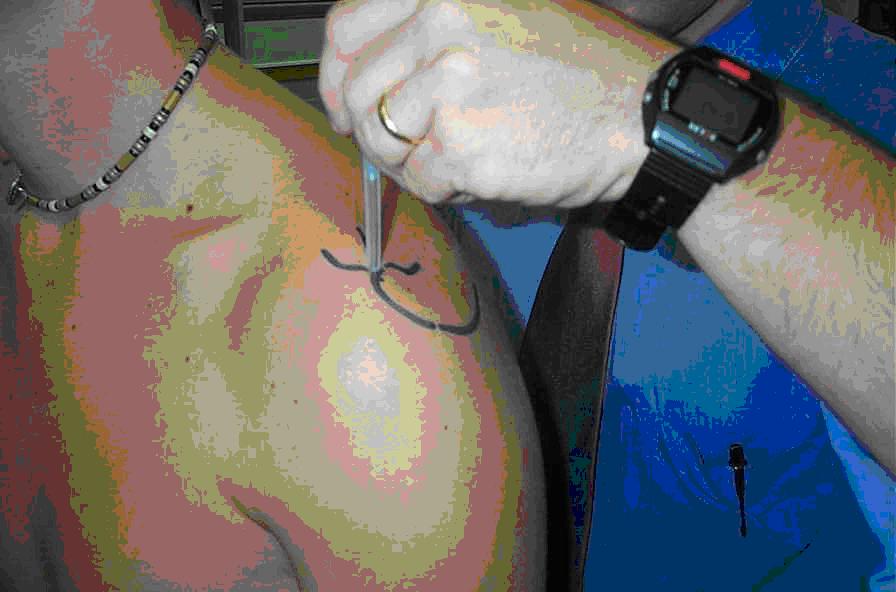
Fig. 2. Injection into the acromioclavicular joint
