No more shin splits!
Shin and leg pain which occurs with exercise and other physical activity is very common. Shin pain comprises up to 12% of all sports injuries, affecting almost 30% of runners and a third of those in military training.
The name for shin pain was previously ‘shin splints’. This is an unhelpful term and is not a diagnosis. When diagnosing shin pain, we need to establish whether it is from a localised problem or referred from another area. In the latter, it is relatively common to suffer shin or leg pain which is referred from the lower back (e.g. sciatica, pinched nerve).
Also, there are some circulation disorders which may cause exercise-related shin or leg pain. This is known as claudication, and it is due to narrowing of the blood vessels to the leg, usually due to atherosclerosis (disease of the arteries).
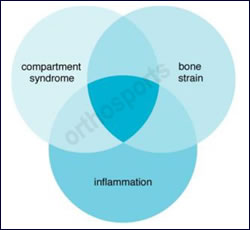
Often there is an overlap of different causes of shin pain. The pain may be muscular, from the bone, or from the lining of the bone. Occasionally, problems related to nerves or blood vessels being compressed may occur.
The most common cause of shin pain with exercise is muscular. This is sometimes referred to as myofascial pain. It is common in those under 30 years of age and is associated with a recent increase in weight-bearing exercise (e.g. jogging). Another feature of myofascial pain is that it reduces when you have warmed up, but it usually recurs towards the end of physical activity.
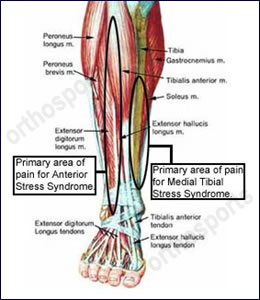
When one or a group of the leg muscles become inflamed and tighten, this may cause other problems affecting the muscle attachment on the bone. This is usually the main bone in the leg, the tibia, and this condition is known as medial tibial stress syndrome, or tibial periostitis. This does not always improve with warming up and impact may cause a sharper pain which is pin-point.
Some researchers believe that tibial periostitis may lead on to a more serious condition affecting the bone, known as a stress fracture. A stress fracture is a failure of bone strength. Microscopic cracks and weakness in the bone cause pain and an inability to tolerate load and impact. Some mild stress fractures only cause pain at the end of exercise. A more severe stress fracture of the tibia typically causes pain when walking, it is worse with exercise, there is pin-point tenderness on the bone, and sometimes there is pain in the leg when lying in bed at night.
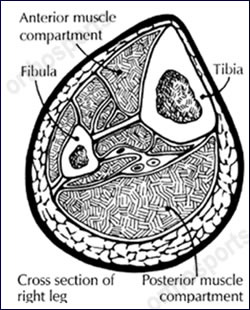
The final condition which is seen regularly in sports medicine clinics is known as compartment pressure syndrome. This is a very interesting condition, where there is an increase in pressure which builds up within certain muscle groups within the leg. Under normal circumstances, when a muscle is active it expands comfortably. Compartment pressure syndrome is a condition where the muscle is unable to expand due to severe tightening of the muscle lining (muscle fascia). The pain is worse with exercise and is not relieved until rest occurs. Other symptoms such as numbness in the leg or foot, a feeling that the leg is becoming rock hard and sometimes discolouration may occur. This is more common in those over the age of 30 years and is common in both legs (bilateral).
Diagnosis
The majority of cases are diagnosed on clinical grounds, that is, the history of the condition and a physical examination, preferably after exercise. Investigations such as X-rays, bone scans or MRI scans are indicated if bone stress is being considered. Compartment pressure testing is a conclusive test to diagnose compartment pressure syndrome.

Bone scan of a tibial stress fracture

MRI scan of a tibial stress fracture
Management
Once a diagnosis is made, a treatment programme may be instituted. Training should be altered to avoid aggravating the condition (eg cycling instead of running). Muscular conditions and mild cases of compartment syndrome may respond to physical treatment, which includes deep tissue massage, strengthening exercises, and stretching exercises. A sports physiotherapist is valuable in this area.
Depending on the degree of bone stress, some stress fractures require the use of a pneumatic brace (e.g. air cast boot) and/or crutches. Severe cases of compartment pressure syndrome require surgery which is known as a ‘compartment pressure release’.
Assessment of footwear and the biomechanics of the feet is helpful and orthotic devices from a sports podiatrist may be required.
The correct diagnosis of exercise-related shin pain is best made early to avoid delays in treatment or aggravation of the condition.