Inside This section
Frozen Shoulder
A frozen shoulder (ADHESIVE CAPSULITIS) is a common condition affecting 3% of the population. It most usually affects people over the age of 40 years, in women far more often than in men. It may be triggered by an injury or previous surgery (heart or breast) but it is also associated with a range of medical conditions including diabetes, thyroid disease, Parkinson’s disease and inflammatory disorders. It occurs in both shoulders in 10% of individuals.
This condition is characterised by specific phases which overlap. Overall though, frozen shoulder is a self-limiting condition which may take up to up to two years to resolve.
There are 3 distinct phases to a frozen shoulder:
- The FREEZING PHASE lasts about 2 to 9 months (sometimes even longer in diabetics). Patients get pain at rest, with activity and also pain at night. There is significant restriction of motion.
- The FROZEN PHASE displays progressive stiffness, lasting up to 12 months. Pain occurs only at the extremes of movement but the shoulder remains stiff.
- The THAWING-OUT PHASE is the resolution phase where movements improve over a 12 to 24 month period. This phase is not typically painful.
In 80% of patients the pain resolves completely but some people are left with a small and permanent restriction of range of motion. This loss of motion does not usually cause any long term problems.
The cause of frozen shoulder is unknown, but some other shoulder conditions may present in a similar manner. These include osteoarthritis, shoulder impingement and calcium deposits. An x-ray is always recommended in the assessment of the stiff, painful shoulder.
To view an animation of Adhesive Capsulitis please see the video below
Treatment
The most important aspect of the treatment is to understand that this is a condition that should get better by itself. The mainstay of treatment is to use the shoulder as much as possible (within the limits of your discomfort). It is important to avoid immobilising the arm or stop using it as this will cause the condition to deteriorate.
Medications have a role and these include analgesics, anti-inflammatories and sometimes medications to assist with sleeping. There is a large range of medications which vary in their effect between individuals. We strongly recommend that you see your family doctor for appropriate medication advice. Cortisone (steroid) injections into the joint are an option but may offer short term relief at best with the added risk of introducing an infection into the joint. These injections are usually given by a Radiologist and using a sterile technique.
Physiotherapy has a role depending on the phase of the frozen shoulder. Exercises are instructed to maintain movement and strength. These should not be painful. The exercises are not designed to improve the range of your movement. The aim of the exercises is to keep the shoulder mobile and avoid further stiffness. Aggressive and painful manipulation of the shoulder may aggravate the condition and should be avoided. It is only necessary to see the physiotherapist on a few occasions and then you should perform the exercises yourself (perhaps 4 times a day, for 5 minutes each time).
There is a relatively new injection technique available called Hydrodilatation (hydrodistension). This is explained further in this document.
In most cases individuals learn to live with the condition for 12 to 24 months – (providing the pain in tolerable and you can cope with the activities of daily living). If you have not reached the “frozen” phase within 9 to 12 months, then there is a reasonable case to perform a Manipulation under Anaesthetic and an injection of cortisone. This requires an admission to hospital for a few hours and a general anaesthetic.
The shoulder is manipulated and injected with cortisone under sterile conditions. Following the procedure you will require 3 to 4 months of physiotherapy. The success rate of the procedure is 70% but there is a 2% chance of breaking your arm during the manipulation. The other risks are those of the anaesthetic and infection into the joint with the injection.
Hydrodilatation and Post-Injection Stretching
HYDRODILATATION (also called hydrodistension) AND POST-INJECTION STRETCHING is an injection and stretching technique where a Radiologist “blows up” or distends the shoulder joint with fluid, and breaks down the contractures. The aim is to advance the patient more quickly through the stages of frozen shoulder.
A number of studies have shown improved movement and pain reduction but there are no good published studies in the medical literature confirming long term improvement. We are involved in two clinical trials at the moment.
The aim of the procedure is to break the cycle of inflammation and contraction of the shoulder joint capsule (capsular fibroplasia).
The procedure involves:
- An injection of up to 50 ml of fluid (some studies have used an even greater volume). This fluid is a combination of cortisone anti-inflammatory, local anaesthetic and sterile saline. This is done by an experienced radiologist under x-ray control.
- A sensation of stretch or ‘pop’ is desired
- Immediate stretching is commenced and continued until medical review within 4 weeks
The risks and side-effects include post-injection pain (up to 3 days), infection (1:15,000) and allergy (1:100,000).
The regime of post-injection stretching is critical. This involves:
- Using the ‘good’ arm to assist in stretching the injured shoulder
- Immediate assisted active stretching into forward elevation and ER (external rotation) for 20mins
- Post-injection stretching with these movements must continue at home aiming for 5 minutes, four times per day
- Use the shoulder and arm as usual within pain limits. The shoulder should not be nursed.
- A formal review and re-examination is needed within 4 weeks. Formal physiotherapy may recommence then, depending on the physical examination.
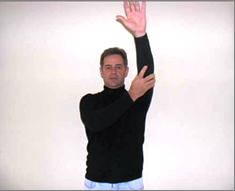
Forward Elevation

Our preliminary results are measured using pain scores, measuring movement and monitoring medication use. Our results are encouraging with good objective and subjective findings. Up to now we have found that:
-
75% patients report a good or excellent overall response
-
95% report reduced pain scores and improved movement
-
100% reduced medication use
-
15% have the injection repeated depending on the symptoms.
Remember, be patient, don’t give up, the condition is self-limiting and there are a range of treatment options available. Further information on the activity of cortisone, research articles and other similar shoulder conditions may be found on our website.
