Home > Teaching > Newsletter > 2006 Newsletter – Winter
2006 Newsletter - Winter
Dear General Practitioners,
Welcome to the Orthosports 2006 newsletter. We know you all have busy practices and find it difficult to keep up with the latest developments in all specialties. Being a subspecialist orthopaedic practice enables us to deliver expert care and keep up to date with the latest advances throughout the world and this newsletter outlines a few of the latest developments.
We have consulting rooms at Randwick, Burwood and Hurstville and operate in a number of private and public hospitals throughout Sydney. We have well respected sports physicians in the practice as well as having physiotherapy and radiology facilities at each site to minimize travel time for patients.
Our website is continuing to grow. It is constantly updated and includes common conditions, surgical procedures and many of our recent lectures for general practitioner education. We are getting over 45000 page hits per month and have had a great deal of positive feedback. If you or your patients have questions regarding any topic it will most likely be found on this site. There is also an education section for your perusal with a number of lectures we have given over the last few years. We welcome any feedback regarding our practice or the web site.
Computer Navigated Total Knee Replacements
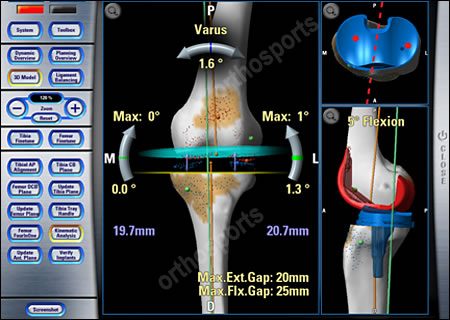
Computer navigated surgery is becoming more popular in knee replacement surgery. It has several proven advantages primarily improved accuracy.
Dr Bruce and Dr Walker have just completed a study showing it is also probably safer. When routine knee replacements are performed rods are put in the canals of the femur and tibia. This causes fat particles to be pushed into the heart, lungs and sometimes the brain if there is a right to left heart shunt.
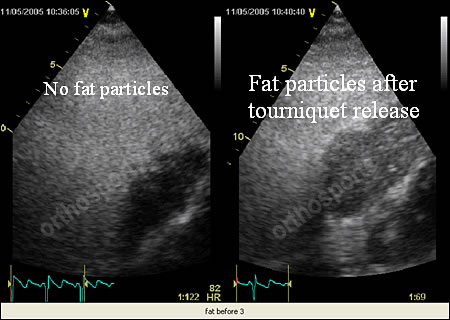
Dr Bruce and Dr Walker have measured the amount of fat that enters the lung using an intraoperative cardiac Doppler technique. They compared the amount of fat emboli in routine knee replacements to those done using a computer navigation technique which doesn’t use any rods in the canals.
The results showed that there were statistically less fat emboli entering the heart using computer navigation. The hypothesis this leads to is that this will result in less stress to the heart, less postoperative confusion and quicker recovery.
Hemicap Device For
Focal Cartilage Defects In The Knee
Dr Craig Waller
The HemiCAP contoured articular prosthesis is an exciting new development in the treatment of focal cartilage defects and early osteoarthritis in the knee.The HemiCAP implant is designed to resurface the affected part of the joint in a precise anatomical manner. This unique system allows the articular contour to be mapped intra-operatively and then replaced with a matching implant.
The HemiCAP implant is made of a material which has proven to provide a safe, effective and strong weight-bearing surface in joints. This metal alloy exhibits lubricious qualities very similar to articular cartilage when implanted in a joint.
Patients with a painful focal articular cartilage defect on the femoral condyle in the knee who are unsuitable for other types of surgery can be successfully treated with this implant. Some patients with early focal osteoarthritis may also be suitable.
Patients often report an almost instant improvement in symptoms “like filling a hole in a tooth” following this procedure, which can be done on an outpatient basis in a day surgery unit.
In some cases of single compartment osteoarthritis, the HemiCAP implant may be an alternative to unicondylar or total knee replacement.

The HemiCAP


HemiCAP device in medial femoral condyle
B.Med., Dip. Sports Med. (London), F.A.C.S.P. Conjoint Lecturer, University NSW
PW: Welcome back from London. John what did you do over there?
JB: Thanks Pete. My family and I lived in London for a little over a year where I worked as a Consultant Sports Physician with the Pure Sports Medicine Group. This was a ‘working sabbatical’ and involved clinical consulting in a multi-disciplinary sports medicine practice, an involvement with a range of teams as a consultant or team doctor and a significant commitment to teaching and training colleagues.
PW: What types of professional experiences were different?
JB: There are only 12 clinicians involved in full-time sports medicine practice in the UK compared with over 100 in Australia. With the vast number of professional teams the UK this creates a high demand and many opportunities. As such I was able to run clinics at clubs, perform medical audits of high performance units and provide input into screening and profiling athletes and team doctoring. I also had the privilege of being keynote speaker at two International Conferences last year – in Dublin and also at the English Institute of Sport.
PW: Sounds busy. What teams were you involved with?
JB: I was involved with Fulham and Charlton Athletic in the English Premier League; Wasps, Bath, Leicester and London Irish in Rugby; London Broncos RL. I also was involved with motor racing, triathlon and performing arts groups. As a ’one-off’ I enjoyed the privilege of being team physician for the Southern Hemisphere Rugby Team in their Tsunami Disaster Fund-raising match (and we had a good win!)
PW: Thanks John, it’s good to have you back. To finish up – have you changed your practice at all?
JB: I have. The 3 main changes are in my assessment of groin pain especially hip impingement syndromes; autologous blood injections for the treatment of chronic tendinopathy (mainly lateral epicondylosis) and exercise prescription for primary and secondary disease prevention. I’m happy for any of our readers to contact me about any of these points.
The trochanteric bursa is located around the gluteal muscles that attach to the greater trochanter at the upper end of the thigh. Trochanteric bursitis is more common in middle-aged or elderly women but can occur in anyone and more often than not has no obvious cause.
Symptoms of trochanteric bursitis include hip pain and tenderness localized to the greater trochanter. The pain can radiate laterally as far as the knee and be worse during activities such as walking, running, or sitting cross-legged. It is often aggravated by lying on the affected side and can wake the patient. The patient may also notice mild swelling and develop a limp.
Treatment for bursitis includes rest and Ice packs to the affected area, simple analgesics or anti-inflammatory medications and weight loss. Physiotherapy is an important part of treatment involving stretching and strengthening exercises for muscles around the hip. If these do not relieve the pain, local anaesthetic or steroid injections into the bursa may help. Occasionally several injections are required. Surgery is a last resort but may occasionally be recommended.
Injection Technique – mix a corticosteroid (such as Celestone) with local anaesthetic (1% lignocaine) in a 10ml syringe. Mix and inject using aseptic techniques with a blue or green (21,23G) needle. Spread the injection over an area of 3 to 5cm without withdrawing the needle totally from the skin, i.e., withdraw slightly and redirect the needle 2 or 3 times. This can be done in your consulting rooms and does not require x-ray guidance. The effects usually take 24-48 hours to work. For the first day or two there can actually be a slight increase in pain as the corticosteroid starts to work. The effects can last anywhere from a week to 6 months but it is only temporary. The injection can be repeated if required (up to three a year).

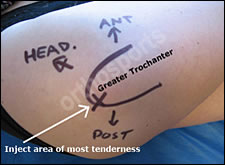
Contraindications include suspected infection, immunosuppression and allergy to local anaesthetic or steroids. Side Effects are rare and include the risk of infection (very low at 1 in 5000), skin discoloration, fat necrosis, flare up of symptoms for a day or two, a rise in sugar levels in diabetics – levels should be monitored carefully for two days.
Meeting of the American
Orthopaedic Foot & Ankle Society
Dr John Negrine
There were interesting lectures presented on Diabetes and the Foot and the increasing role of obesity in American society is causing diabetes and therefore causing foot problems.
The use and abuse of MRI was another topic for discussion. Much MRI scanning in the foot and ankle is inappropriately ordered and as in many other areas in the body, there were numerous false/positives.
There was much discussion regarding Fosamax and the fact that Fosamax resides in the fat particularly in young women for at least 10 years and that great caution was recommended in prescribing this to young people with regard to teratogenic effects. Of interest is that there are lawyers in the US touting for business with people who have taken Fosamax and developed avascular necrosis of the jaw.
Osteoarticular allograft (using a cadaver lower tibia and proximal talus) for people with post-traumatic arthritis of the ankle was another interesting paper. The results of this procedure have been dismal in the past and a recent study presented by a group in Baltimore has once again showed dismal results for this problem. In a young person an ankle arthrodesis is still the procedure of choice when the patient develops post traumatic arthritis
Dr Warwick Bruce – HIP AND KNEE
M.B., B.S.(Syd), F.I.C.S., F.R.A.C.S., F.A. Ortho. A.
Fellowships in Sports medicine and reconstructive hip and knee surgery. Travelling fellow in USA in joint replacement surgery. He consults at all Orthosports rooms ,operates at Calvary Hurstville Community Hospital, Canada Bay Private Hospital and Concord Hospital. He has published and written extensively and has been on the design team for hip and knee replacements.
Dr Jerome Goldberg – SHOULDER
M.B., B.S., F.R.A.C.S., F.A. Ortho. A.
Fellowship at the New York Orthopaedic hospital. Special interests include arthroscopic instability and rotator cuff surgery. He consults at all Orthosports rooms, operates at Calvary Hurstville Community Hospital, Canada Bay Private Hospital and Prince of Wales Private Hospital.
Dr Andreas Loefler – SPINE, TRAUMA, HIP AND KNEE
B.S.C., M.B., B.S., F.R.A.C.S. (Ortho.)
Anzac travelling fellowship of the Australian Orthopaedic Association. He consults at the Hurstville and Randwick rooms and operates at Calvary Hurstville Community Hospital, Prince of Wales Private and Public Hospitals.
Dr John Negrine – ADULT FOOT AND ANKLE
M.B., B.S. (Syd), F.R.A.C.S.
Sydney Orthopaedic trained. US accredited Fellowship in foot and ankle surgery at Baylor University Medical Centre, Dallas Texas 1994. Member Australian, American and European Foot and Ankle Societies. He consults at all three Orthosports rooms and operates at Prince of Wales Private Hospital, Canada Bay Private Hospital and Calvary Hurstville Community Hospital.
Dr Rodney Pattinson – PAEDIATRICS
M.B.B.S (1983) F.R.A.C.S (Ortho.)
Fellowship at the Hospital for Sick Children in London and Princess Margaret Rose Hospital in Edinburgh. He also operates on adults with hip and knee conditions. He consults at all Orthosports rooms, operates at Canada Bay Private Hospital and Sydney Children’s Hospital and St George Hospital.
Dr Ivan Popoff – SHOULDER, KNEE AND ELBOW
BPhEd(1987), MBChB(1991), F.R.A.C.S. (Ortho.)
Fellowship in Sports Medicine, Shoulder and Knee Surgery, Dalhousie University, Halifax NS Canada. He consults at all the Orthosports rooms and operates at Calvary Hurstville Community, Prince of Wales Private and Canada Bay Private Hospitals.
Dr Doron Sher – KNEE, SHOULDER AND ELBOW
M.B., B.S. (NSW), M.Biomed.E., F.R.A.C.S. (Ortho.)
Fellowships in upper and lower limb surgery. Sports Medicine Knee and Shoulder Surgery- Canada, Elbow surgery-Mayo Clinic, Upper Limb Surgery- New York. He consults at the Randwick and Burwood rooms and operates at Prince of Wales Private, Concord Public and Canada Bay Private Hospitals.
Dr Allen Turnbull – HIP AND KNEE
M.B., B.S. (1980), F.R.A.C.S. (Ortho. 1988)
Fellow in joint replacement surgery. Interest in sporting injuries involving the knee and joint replacement. He consults at the Hurstville office. He operates at Calvary Hurstville Community Hospital, Kareena and St George Private Hospitals and St George Public Hospital.
Dr Peter Walker – HIP AND KNEE
M.B., B.S. (Hons 1990), F.R.A.C.S. (Ortho.)
Awarded Zimmer travelling fellowship.Two accredited fellowships in hip and knee surgery in Boston and Toronto. He consults at the Burwood and Randwick rooms and operates at Canada Bay Private Hospital, Prince of Wales Private, Concord and Canterbury Public Hospitals.
Dr Craig Waller – HIP AND KNEE
M.B., B.S. (Hons, NSW 1982), F.R.C.S. (Ed.), F.R.A.C.S. (Ortho. 1989)
He was awarded the University medal and graduate prize in surgery. He consults at the Burwood and Randwick rooms and operates at Canada Bay Private Hospital and Prince of Wales Private Hospital.
Sports Medicine
Dr John Best
B.Med., Dip. Sports Med. (London), F.A.C.S.P.
Sports Physician
Dr Hugh Hazard
M.B., B.S., Grad. Dip. Sp. Science, F.A.C.S.P.
Sports Physician
Dr Mel Cusi
M.B., B.S., Cert. Sports Medicine (RACGP), F.A.C.S.P.
Sports Physician
Dr Angus Bathgate
M.B., B.S.
Sports Physician
Dr Paul Annett
M.B., B.S. (Hons. I), F.A.C.S.P.
Conjoint lecturer UNSW
