Question for Physiotherapists

NRL head injury management
Welcome to Orthosports Question for Physiotherapists June 2025. This month Dr Paul Annett discusses the NRL decision making behind the head injury process.
REMINDER: SAVE THE DATE Orthosports Annual Orthopaedic Updates, Saturday, 8th November, 2025, live @UNSW or via webinar. Registrations open later in the year.
If you have a Question that you would like answered on this monthly email please send to education@orthosports.com.au
QUESTION | I have been watching the NRL and am interested in the decision making process behind the head injury process. Could you explain it to me?
The NRL initiated the ISB (Injury Surveillance Bunker) just prior to the 2022 season. It was introduced to ensure the safe and accurate management of in game head injury, improving the immediacy of player removal from the field for head trauma and assisting the Club Medical Officer (CMO) in the management of game day concussion. One of the predictors of outcome and recovery is the rapid diagnosis of a concussion event, and a prompt removal of a player from the field as quickly as possible. Any delays in these steps gives less favourable outcomes.
I have been working in the ISB from its commencement, along with Dr John Best and Dr Leigh Golding, and a collection of other Sports Physicians and experienced sports doctors.
The purpose of the ISB is to use detailed video analysis to determine potential severity of an in-game head trauma or concussive force transmitted to the head. It is a system purely based on video signs noted and not a definitive diagnosis of concussion, which must be made with an accurate clinical assessment by the CMO. This is not to be confused with simply observing a heavy tackle or impact between players, which may look spectacular, but does not lead to clear video signs of concussion and mandate player removal from the field.
Logistically the ISB is located in a television studio in Redfern in Sydney, in conjunction with the video referee bunker. The ISB is made up of 5 people. There is a medical officer, 2 ‘spotters’ and 2 technical supports. The spotters are experienced and well-trained rugby league people (ex-players, physiotherapists, exercise physiologists). One spotter’s job is to watch the game continually and ‘tag’ any potential head impacts for more detailed analysis. These incidents will then be further scrutinized, with the second spotter and 1 of the technical supports providing the best of a series of multiple video angles (up to 12 camera angles), delivered to the medical officer, who ultimately decides whether the incident requires a classification or is deemed non-significant. In any one game of rugby league there may be numerous incidents of contact around the head, most of which do not require categorization. The second technician communicates with a sideline assistant at the ground, where there is video set-up for the CMO to review any incidents that occur. CMO review of the video footage is mandatory for any reportable incidents.
There are 2 main classification groups that the ISB works with – a Category 1 and a Category 2 concussion.
Category 1 signs indicate that the player has concussion and must be immediately removed from the field. They are not to be allowed to return to play on that day, irrespective of symptom recovery during the game.
Category 1 signs include:
- Lying motionless (suspected loss of consciousness)
- Motor incoordination (ataxia or stumbling)
- Impact seizure
- Tonic posturing
- Lack of protective Action (Player becomes floppy)
- Blank or vacant look
Category 2 signs indicate the potential for concussion. When identified the player must be removed from the field and taken for a SCAT 6 assessment by the CMO. If the player passes this within an allocated 15minute time-frame, then they are free to return to the field of play.
Category 2 signs include:
- Lying motionless (>2, but <5 seconds) in the context of a head injury (possible LOC)
- Possible impact seizure
- Possible tonic posturing
- Possible motor incoordination
- Slow to stand (15 seconds)
In addition, if it is noted that the player doesn’t look right, looks dazed, shakes head, opens and closes eyes quickly, this may indicate category 2 symptoms.
A category 3 has also been devised which is designated as a ‘trainer check’. In these cases, there may have been a significant head impact although without clear category 1 or 2 signs. The ISB will ask the CMO to have the orange shirt trainer perform an on-field assessment of the player. If there are any concerns (such as failing orientation or Maddocks questions or any disturbance of balance) then the player can be upgraded to a category 2 by the trainer and removed for a SACT 6 assessment.
It has been determined that over the last 3 years the introduction of the ISB has led to a more rapid removal of players from the field. This is particularly for category 2 incidents where the player will be regularly removed in under 60 seconds. From a personal perspective the ISB has been a worthwhile initiative. I can recount numerous incidents, particularly in category 2 concussion, where both the head contact and subsequent signs were sufficiently obscured only to be noted on a single camera angle, which ultimately led to a player being removed from the field and subsequently failing the SCAT 6 assessment. As a result, there has been a clear improvement in the level of player safety with respect to immediate concussion management and potentially reducing the likelihood of developing long term issues such as CTE (chronic traumatic encephalopathy).


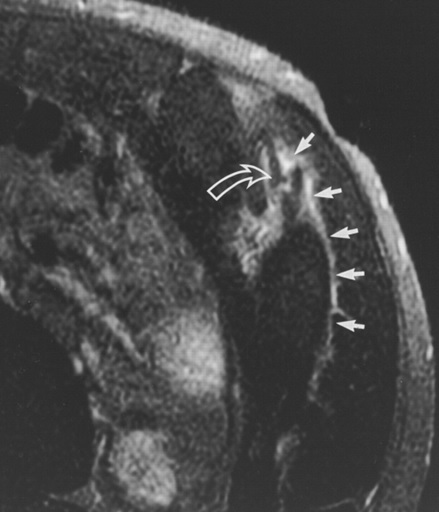
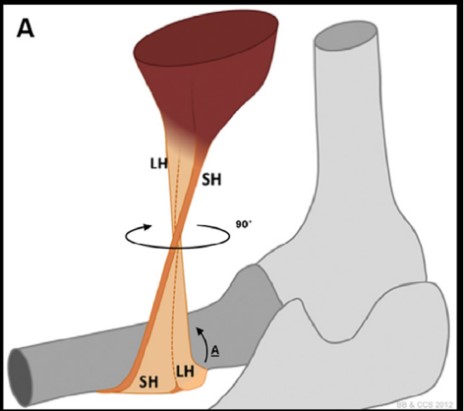
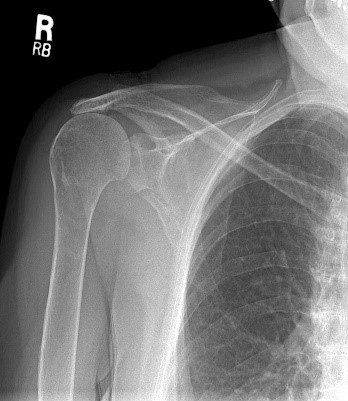
Internal Impingement of the Shoulder
Welcome to Orthosports Question for Physiotherapists May 2025. This month Dr Leigh Golding discusses internal impingement of the shoulder. REMINDER: SAVE THE DATE Orthosports Annual Orthopaedic Updates, Saturday, 8th

Swollen Ankle
Welcome to Orthosports Question for Physiotherapists April 2025. This month Dr John Negrine discusses a swollen ankle. REMINDER: SAVE THE DATE Orthosports Annual Orthopaedic Updates, Saturday, 8th November, 2025,
Glenoid track and shoulder instability scoring system
Welcome to Orthosports Question for Physiotherapists March 2025. This month Dr Doron Sher gives an update on the glenoid track and shoulder instability scoring system. Do you

Spontaneous Osteonecrosis
Welcome to Orthosports Question for Physiotherapists September 2024. This month Dr Doron Sher discusses Spontaneous Osteonecrosis. REMINDER TO REGISTER Orthosports Annual Orthopaedic Updates, Saturday, 9th November 2024, Live event
Side Strain
Welcome to Orthosports Question for Physiotherapists August 2024. This month Dr Leigh Golding discusses side strain from a sporting injury. REMINDER: SAVE THE DATE Orthosports Annual Orthopaedic Updates, Saturday,

Tarsal coalition
Welcome to Orthosports Question for Physiotherapists July 2024. This month Dr Paul Annett discusses Tarsal coalition. REMINDER: SAVE THE DATE Orthosports Annual Orthopaedic Updates, Saturday, 9th November 2024, live

Patella dislocation
Welcome to Orthosports Question for Physiotherapists May 2024. This month Dr Doron Sher discusses Patella dislocation SAVE THE DATE: Orthosports Annual Orthopaedic Updates, Saturday, 9th November 2024, live

Gout
Welcome to Orthosports Question for Physiotherapists April 2024. This month Dr John Negrine discusses the common condition of Gout. SAVE THE DATE: Orthosports Annual Orthopaedic Updates, Saturday, 9th
Distal Biceps Rupture
Welcome to Orthosports Question for Physiotherapists February 2024. This month Dr Doron Sher discusses management of distal biceps rupture. If you have a Question that you

Sport after Total Knee Replacement
Welcome to Orthosports Question for Physiotherapists, October 2023. This month Dr Doron Sher discusses return to sport after total knee replacement. REMINDER: Register your place for the Annual Orthopaedic Updates.

High Tibial Osteotomy and Uni Knee Replacement
Welcome to Orthosports Question for Physiotherapists, September 2023. This month Dr Doron Sher discusses the comparison of the High Tibial Osteotomy vs the Unicompartmental Knee Replacement. Register your
Achilles Tendon Ruptures
Welcome to Orthosports Question for Physiotherapists, August 2023. This month Dr John Negrine discusses Achilles Tendon Ruptures. Save the Date: Saturday, 4th November, 2023 Annual Orthopaedic Updates. Live

Lateral extra-articular tenodesis
Welcome to Orthosports Question for Physiotherapists, June 2023. This month Dr Michael Goldberg discusses lateral extra-articular tenodesis and why you would add this procedure to an ACL
Adding a Patch to Rotator Cuff Repairs
Welcome to Orthosports Question for Physiotherapists, May 2023. This month Dr Doron Sher discusses the use of a patch in Rotator Cuff Repairs. Save the Date: Saturday, 4th

Imaging for ACL Injury
Welcome to Orthosports Question for Physiotherapists, October 2022. This month Dr Doron Sher discusses imaging for a suspected ACL injury. Save the Date: Saturday, 12 November, 2022 Annual
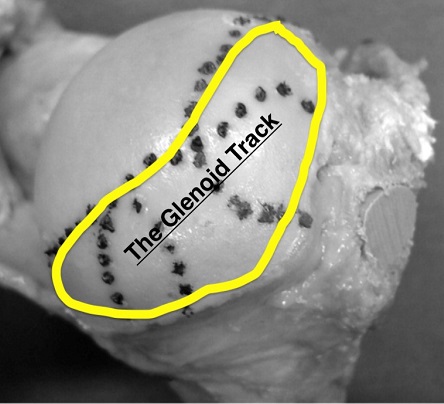
Glenoid Track and Shoulder Instability
Welcome to Orthosports Question for Physiotherapists August, 2022. This month Dr Doron Sher discusses a question on the glenoid track and shoulder instability. Please send your Questions

OSTEOCHONDRITIS DISSECANS
Welcome to Orthosports Question for Physiotherapists May, 2022. This month Dr Doron Sher discusses a question on treatment options for an OCD Lesion. Save the Date: Saturday,
Accessory Bones of the Foot and Ankle
Welcome to Question for Physiotherapists, April, 2022 This month Dr John Negrine discusses accessory bones of the foot and ankle. Please feel free to send your

Hypermobile Lateral Meniscus
Welcome to Question for Physiotherapists, March, 2022 This month Dr Michael Goldberg discusses the Hypermobile Lateral Meniscus. Please feel free to send your questions to

Imaging in Musculoskeletal assessment
Welcome to Question for Physiotherapists, February, 2022 This month Dr Paul Annett discusses Imaging inMusculo-skeletal Assessment. Please feel free to send your questions to education@orthosports.com.au Dr
Shoulder Injury related to vaccine administration
Welcome to Question for Physiotherapists, January, 2022 This month Dr Doron Sher discusses Shoulder Injury related to Vaccine administration. Please feel free to send your questions

Chondral Grafting in the knee
Welcome to Question for Physiotherapists, November 2021. This month Dr Doron Sher discusses Chondral Grafting in the knee.Please feel free to send your questions to education@orthosports.com.au CHONDRAL

Syndesmosis Fixation
Welcome to Question for Physiotherapists, October 2021. This month Dr Todd Gothelf discusses Syndesmosis fixation. Please feel free to send your questions to education@orthosports.com.au QUESTION I

Hip Precautions following Total Hip Replacement
Welcome to Question for Physiotherapists, September 2021. This month Dr Christopher Spelman discusses precautions after a Total Hip Replacement. Please feel free to send your questions
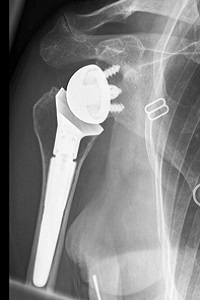
Reverse Shoulder Replacement Rehabilitation
Welcome to Question for Physiotherapists, August 2021. This month Dr Doron Sher discusses rehabilition after a Reverse Shoulder Replacement. Please feel free to send your questions
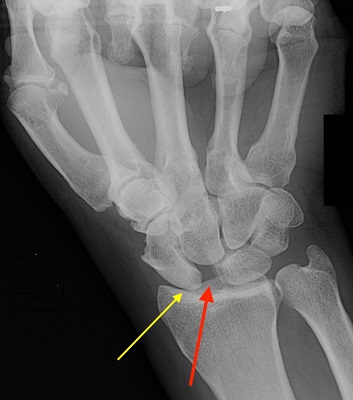
Chronic Scapholunate Ligament Rupture
Welcome to Question for Physios, July 2021. This month Dr Kwan Yeoh discusses the management of Complete Scapholunate Ligament Rupture. Please feel free to send your

Assessing Sports Injury
Welcome to Question for Physiotherapists June 2021. This month Dr Paul Annett presents an article on assessing a patient that presents with potentially more than a

Discoid Lateral Meniscus
Welcome to Question for Physiotherapists May 2021. This month Dr Doron Sher presents an article on a Discoid Lateral Meniscus. Please feel free to send

Cavo-Varus (High Arched) Feet
QUESTION | Why are high arched feet more interesting than flat feet? ANSWER | A 43 year old man presents with numbness on the outer

Surgical Treatment of Unstable Shoulder
QUESTION | | Surgical treatment of the unstable shoulder – How do you decide which patient gets what operation? We know that younger patients and those
Full Thickness Tear of Supraspinatus Tendon
QUESTION | My patient is a 67 year old female who has had pain during overhead activity (catching pain), going on for over 5 years.

Medial Meniscal Root Tears
QUESTION I I have a patient in her 50s who has had a meniscus repair done. I thought that the studies showed no advantage when doing
Wrist Ganglion & Carpal Instability
QUESTION| How Does a Wrist Ganglion relate to Carpal Instability? How is it best treated? ANSWER | A ganglion is a benign synovium-lined cystic collection of

Lumbar Stress Fractures
QUESTIONS | 1. What is rest in treatment of stress fracture? Walking only? Bike? Swim(in non-extended position)? What can you do? Or is it just not
Collateral Ligament Tear
QUESTION | WHEN DOES A COLLATERAL LIGAMENT TEAR OF THE THUMB NEED SURGERY? ANSWER | For the purposes of this question, I’m going to assume
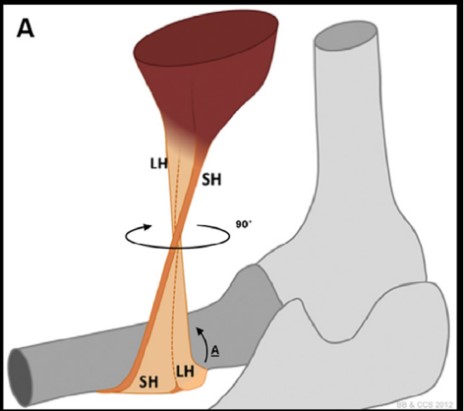
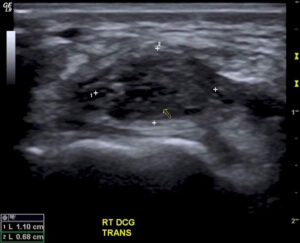
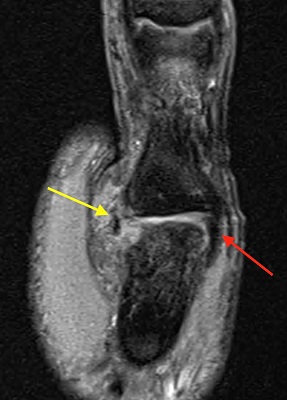
Distal Biceps Rupture
QUESTION | I recently had a patient with a partial distal biceps rupture. Why was he offered surgery without trying non-operative management? ANSWER | Anatomy:

Hallux Rigidus
QUESTION | What are the best options for a 50 year old runner with Hallux Rigidus? ANSWER | A 50 year old runner with hallux
Previous Question for Physiotherapists:
| Dec-2020 | Wrist Ganglions | Dr Kwan Yeoh |
| Oct/Nov-2020 | Medial Meniscal Root Tears | Dr Doron Sher |
| Sep-2020 | Lumbar Stress Fractures | Dr Paul Annett |
| Aug-2020 | Frailty and Healthy Ageing | Dr John Best |
| Jul-2020 | Thumb – Collateral Ligament Tear | Dr Kwan Yeoh |
| Jun-2020 | Shoulder Instability | Dr Doron Sher |
| May-2020 | Hallux Rigidus | Dr John Negrine |
| Mar/Apr-2020 | Achilles Tendon Ruptures | Dr Todd Gothelf |
| Feb-2020 | Distal Biceps | Dr Doron Sher |
| Nov-2019 | Clavicle Fracture Internal Fixation | Dr Doron Sher |
| Oct-2019 | Femoracetabular Impingement (FAI) | Dr Paul Mason |
| Sep-2019 | Imaging for Acute ACL Injuries | Dr Doron Sher |
| Aug-2019 | Joint Relocation | Dr Paul Annett |
| Jul-2019 | Guyon canal surgery | Dr Kwan Yeoh |
| Jun-2019 | Whats new in ACL reconstruction 2019 | Dr Doron Sher |
| May-2019 | Cuneiform Fracture | Dr Todd Gothelf |
| Apr-2019 | Flexor Tendon Injuries | Dr Kwan Yeoh |
| Mar-2019 | Chronic Exertional Compartment Synd | Dr Paul Annett |
| Feb-2019 | Achilles Tendon Rupture | Dr John Negrine |
| Nov-2018 | Low Back Pain | Dr Paul Mason |
| Sep-2018 | Concussion part 2 | Dr John Best |
| Jul-2018 | Concussion part1 | Dr Paul Annett |
| Jun-2018 | Thessaly & McMurray Test | Dr Doron Sher |
| May-2018 | AC Joint | Dr Doron Sher |
| Apr-2018 | Arthritis of the fingers | Dr Kwan Yeoh |
| Feb-2018 | CLAVICLE fractures | Dr Doron Sher |
| Oct-2017 | ACL Grafts | Dr Doron Sher |
| Sep-2017 | Forefoot pain | Dr John Negrine |
| Aug-2017 | Wrist Ganglion | Dr Kwan Yeoh |
| Jul-2017 | Anterolateral Ligament Reconstruction | Dr Doron Sher |
| Jun-2017 | Scapholunate ligament | Dr Kwan Yeoh |
| Apr-2017 | Knee Brace – ACL Reconstruction | Dr Doron Sher |
| Mar-2017 | Sesamoid fractures | Dr Kwan Yeoh |
| Feb-2017 | Plantar Fasciitis | Dr Todd Gothelf |
| Nov-2016 | Sternoclavicular Joint | Dr Doron Sher |
| Oct-2016 | Proximal Humerus Fractures | Dr David Lieu |
| Sep-2016 | Wrist Fractures | Dr Kwan Yeoh |
| Aug-2016 | Patella Instability | Dr Doron Sher |
| Jul-2016 | Snowboarders ankle | Dr Todd Gothelf |
| May-2016 | Cortisone Injections | Dr Paul Annett |
| Apr-2016 | Shoulder Instability_1 | Dr Ivan Popoff |
| Mar-2016 | Exercise after TKR | Dr Doron Sher |
| Dec-2015 | Scaphoid OA | Dr Kwan Yeoh |
| Nov-2015 | Greater Tuberosity Fractures | Dr Doron Sher |
| Oct-2015 | Stress Fractures | Dr Paul Annett |
| Sep-2015 | Boxers Fractures | Dr Kwan Yeoh |
| Aug 2015 | Resistance Training | Dr John Best |
| July 2015 | LARS Ligament | Dr Ivan Popoff |
| Jun-2015 | Distal Biceps | Dr Doron Sher |
| May-2015 | Latarjet procedure | Dr Jerome Goldberg |
| Apr-2015 | TFCC Questions | Dr Kwan Yeoh |
| Mar-2015 | Acute Ankle Sprains | Dr Todd Gothelf |
| Nov-2014 | PRPP | Dr Paul Annett |
| Oct-2014 | Driving After Surgery | Dr Doron Sher |
| Sep-2014 | Distal Biceps Rupture | Dr Doron Sher |
| Aug-2014 | Ankle Sprain | Dr Todd Gothelf |
| Jun-2014 | Patella Dislocation | Dr Doron Sher |
| May-2014 | Shoulder Instability | Dr Todd Gothelf |
| Apr-2014 | De Quervains | Dr Kwan Yeoh |
| Mar-2014 | Acromio-clavicular joint injuries | Dr Todd Gothelf |
| Feb-2014 | Chronic Knee Pain | Dr Paul Annett |
| Dec-2013 | Foot and Ankle Questions | Dr John Negrine |
| Oct-2013 | Rotator Cuff Repair | Dr Todd Gothelf |
| Sep-2013 | ACL Reconstruction | Dr Doron Sher |
| Jul-2013 | Slipped Upper femoral epiphysis | Dr Rod Pattinson |
| May-2013 | Skiers thumb | Dr Kwan Yeoh |
| Apr-2013 | Bakers_Cyst | Dr Ivan Popoff |
| Mar-2013 | Tibial Osteotomy vs UKR | Dr Doron Sher |
| Feb-2013 | ALIF success rate | Dr Andreas Loefler |
| Jan-2013 | Lisfranc Injuries | Dr Todd Gothelf |
| Nov-2012 | Anterior Spinal Fusions | Dr Andreas Loefler |
| Oct-2012 | MCL Injuries | Dr Doron Sher |
| Sep-2012 | Compartment Syndrome | DrPaul Annett |
| Aug-2012 | Carpal tunnel | Dr Kwan Yeoh |
| July-2012 | Anterior Process Calcaneus Fx | Dr Todd Gothelf |
| Jun-2012 | Tenodesis vs Tenotomy | DrJeromeGoldberg |
| May-2012 | Osteoarthritis in the young active patient | Dr Doron Sher |
| Apr-2012 | Syndesmosis Sprain | Dr Todd Gothelf |
| Mar-2012 | Triangular Fiocartilage Injuries | Dr Kwan Yeoh |
| Jan-2012 | Shoulder Replacement Older Population | Dr Jerome Goldberg |
| Dec-2011 | Wrist Fracture | Dr Kwan Yeoh |
| Nov-2011 | Adductor Tendon Tear | Dr Paul Annett |
| Oct-2011 | Navicular Pain | Dr Todd Gothelf |
| Sep-2011 | OCD Lesion | Dr Doron Sher |
| Aug-2011 | Metal on Metal Hip Replacements | Dr Andreas Loefler |
| July-2011 | Femoral Neck Stress Fract (Pt 2) | Dr John Best |
| Jun-2011 | Femoral Neck Stress Fractures | Dr John Best |
| May-2011 | PCL Injury Part 2 | Dr Doron Sher |
| Apr-2011 | PCL Injury Part 1 | Dr DoronSher |
| Mar-2011 | Prolotherapy Autologous Blood Injections | DrPaul Annett |
| Feb-2011 | Shoulder Impingement | Dr Todd Gothelf |
| Dec-2010 | Does Chondral Grafting Work | DrDoron Sher |
| Nov-2010 | Shoulder Immobilisation-Dislocation | Dr Jerome Goldberg |
| Sep-2010 | SLAP Lesions Stable Shoulder | Dr ToddGothelf |
| Jul-2010 | Ankle Sprains | Dr Todd Gothelf |
| Jun-2010 | Dislocation After THR | Dr Peter Walker |
| May-2010 | Acupuncture Muscle Strength Programmes | Dr Paul Annett |
| April-2010 | Full Thickness Rotator Cuff Tears | Dr JeromeGoldberg |
| Mar-2010 | Skiing after TKR | Prof Warwick Bruce |
| Feb-2010 | Fractures of the Clavicle | Dr John Trantalis |
| Jan-2010 | Osteoarthritis of the Knee | Dr Doron Sher |
| Dec-2009 | Fifrth Metatarsal Fractures | Dr Todd Gothelf |
| Nov-2009 | Partial Rotator Cuff Tears | Dr Todd Gothelf |

