Question for Physiotherapists

Knee Injuries from bouldering
Welcome to Question for Physiotherapists February 2026. This month Dr Doron Sher discusses Complex Knee Injuries from Bouldering.
Save the Date: 2026 Orthopaedic Update will be held Saturday, 1st August 2026 at UNSW and via webinar.
If you have a Question that you would like us to answer please send your Questions to education@orthosports.com.au
ANSWER |
Bouldering is like rock climbing but done without safety ropes: just you, your shoes and a crash mat. The ‘routes’ up the wall are short but require significant skill and power to complete. As the level of skill in the climbers improves, the height to which they climb increases as well. Heights of 4 or 5 metres can be attained and it is common to fall from this height when attempting more advanced manoeuvres.
It is rare to hurt yourself during a fall while rock climbing as the rope and harness are designed to provide safety to the climber. This is not the case when bouldering and hitting the ground from a height means that your legs and knees usually take the impact.
Traditionally climbing has been associated with upper limb injuries such as shoulder dislocations because the safety rope limits the distance you can fall off the wall. Unfortunately, the falls from bouldering are leading to high-energy ground impacts, particularly with the lower limbs. The resulting injuries can range from mild sprains to severe ligament tears, often from awkward landings, twisting movements, or high-impact falls.
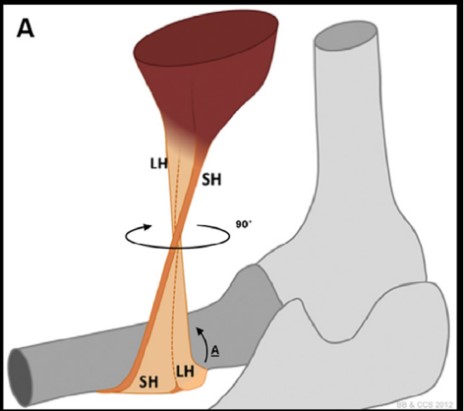
The injury patterns that result from these high-energy axial and rotational loading are often multi-ligament knee injuries with dislocations and complex meniscus tears (including posterior root tears and injuries to both medial and lateral menisci). I have even seen a patella tendon rupture.
Most multi-ligament knee injuries in the past have been from sports like rugby which are very male dominated. Since bouldering has a high number of female participants we are now seeing these severe injuries in the female population as well.
Some common scenarios that cause trouble:
- Jumping off the top instead of downclimbing (even controlled jumps can go wrong)
- Landing on one leg or with your knee twisted
- Rotating the knee under load during heel hooks or drop knees
- Misjudged high steps or awkward shifts in body weight
Mechanisms and Common Causes
An awkward landing is the most common cause of serious injury causing hyperextension or forceful rotation of the knee but the knee can be injured dynamically doing heel hooks, drop knees (ER and loaded) or high stepping. These are usually less serious injuries. Once they have completed the climb many participants choose to jump off the wall rather than climbing back down the way they came. While this can be a controlled landing things can still go wrong jumping from a significant height. Falling off unexpectedly is where the most serious injuries occur.
Types of Knee Injuries
Injuries vary from ACL rupture to a complete posterolateral corner disruption. Meniscal tears are common and it is possible to get chondral injuries as well. I have seen patella tendon ruptures, patella dislocations and MCL strains and disruptions. The most serious knee injuries in bouldering often involve ligament damage.
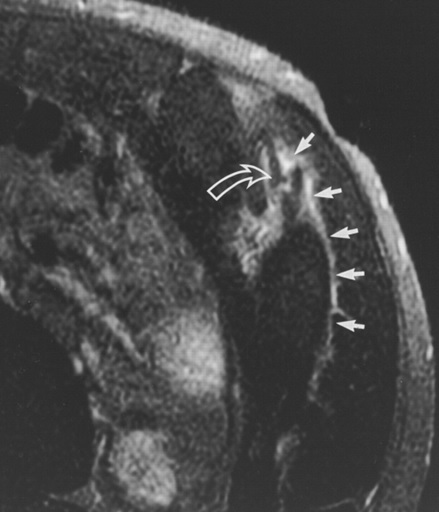
High-energy axial loading that occurs during bouldering falls can lead to meniscus root tears. Given the biomechanical importance of the meniscus root tears (untreated injuries can result in early-onset osteoarthritis), increased vigilance is warranted, particularly when treating female patients with bouldering-related knee injuries because there can be significant articular surface trauma beyond ligamentous and meniscal damage.
This is in contrast to Rock climbing injuries in general.
Spine injuries account for about 5% of all climbing-related injuries and up to 20% of fractures. The majority of these are compression type injuries in the thoracolumbar region sustained by falling from height.
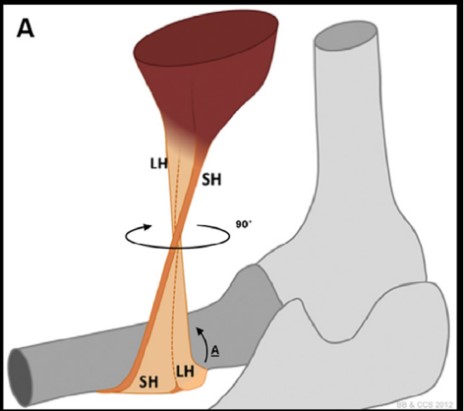
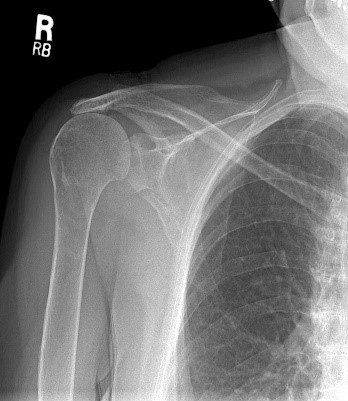
Shoulder injuries are the second most common type in the upper extremity (after the hand). Acute injuries include fractures, acromioclavicular separation, glenohumeral dislocation, and rotator cuff tears. Chronic overuse injuries include rotator cuff tears, impingement, biceps tendonitis, and SLAP tears.
Even first time dislocators are offered surgery as they have a high risk of re-dislocating. Typically an arthroscopic stabilisation and Remplissage procedure will allow them to keep their movement but also remain stable (both of which are essential for climbing).
SLAP tears are also common but often get better with physio. In those that fail non-operative treatment, biceps tenodesis has an almost 100% return to sport rate within 6 months (for high-level competitive rock climbers).
If for some reason the rope does not save you while rock climbing then you are likely to suffer a calcaneal injury or spine fracture.
Conclusion
Bouldering is fun, challenging, and incredibly rewarding — but it also comes with real physical risks, especially to your knees. As climbers push harder and climb higher, injuries from falls are becoming more common, and many of them are serious.
The good news is that most knee injuries in bouldering are preventable. Smart training, proper landing technique, better crash pad use, and education around movement mechanics can all make a huge difference. Jumping off the wall instead of downclimbing, poor landing form, or letting fatigue take over can all lead to avoidable injuries.
As the sport grows, so should our understanding of how to stay safe. Protecting your knees means thinking ahead, respecting your limits, and giving your body the support it needs — whether that’s strength training, recovery time, or just learning to fall well. Protecting their knees should remain a top priority for every boulderer.
Syndesmosis Injury
Welcome to Question for Physiotherapists November 2025. This month Dr John Negrine discusses syndesmosis injury. If you registered for the Orthopaedic Updates Webinar 2025 the recorded webinar will
Acromioclavicular (AC) Joint Injuries
Welcome to Orthosports Question for Physiotherapists October 2025. This month Dr Doron Sher discusses acromioclavicular joint injuries. Reminder to Register Orthosports Annual Orthopaedic Updates, Saturday, 8th November, 2025
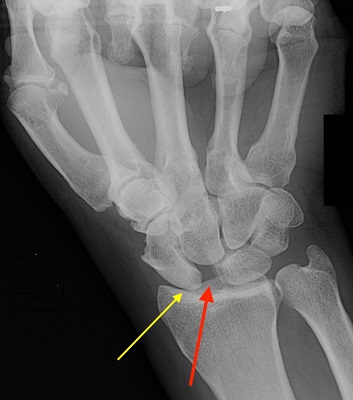
Wrist Fracture Xrays
Welcome to Orthosports Question for Physiotherapists August 2025. This month Dr Kwan Yeoh discusses wrist fractures and xrays. REGISTRATIONS OPEN Orthosports Annual Orthopaedic Updates, Saturday, 8th November, 2025, to register
NRL head injury management
Welcome to Orthosports Question for Physiotherapists June 2025. This month Dr Paul Annett discusses the NRL decision making behind the head injury process. REMINDER: SAVE THE DATE Orthosports Annual
Internal Impingement of the Shoulder
Welcome to Orthosports Question for Physiotherapists May 2025. This month Dr Leigh Golding discusses internal impingement of the shoulder. REMINDER: SAVE THE DATE Orthosports Annual Orthopaedic Updates, Saturday, 8th

Swollen Ankle
Welcome to Orthosports Question for Physiotherapists April 2025. This month Dr John Negrine discusses a swollen ankle. REMINDER: SAVE THE DATE Orthosports Annual Orthopaedic Updates, Saturday, 8th November, 2025,
Glenoid track and shoulder instability scoring system
Welcome to Orthosports Question for Physiotherapists March 2025. This month Dr Doron Sher gives an update on the glenoid track and shoulder instability scoring system. Do you

Spontaneous Osteonecrosis
Welcome to Orthosports Question for Physiotherapists September 2024. This month Dr Doron Sher discusses Spontaneous Osteonecrosis. REMINDER TO REGISTER Orthosports Annual Orthopaedic Updates, Saturday, 9th November 2024, Live event
Side Strain
Welcome to Orthosports Question for Physiotherapists August 2024. This month Dr Leigh Golding discusses side strain from a sporting injury. REMINDER: SAVE THE DATE Orthosports Annual Orthopaedic Updates, Saturday,

Tarsal coalition
Welcome to Orthosports Question for Physiotherapists July 2024. This month Dr Paul Annett discusses Tarsal coalition. REMINDER: SAVE THE DATE Orthosports Annual Orthopaedic Updates, Saturday, 9th November 2024, live

Patella dislocation
Welcome to Orthosports Question for Physiotherapists May 2024. This month Dr Doron Sher discusses Patella dislocation SAVE THE DATE: Orthosports Annual Orthopaedic Updates, Saturday, 9th November 2024, live

Gout
Welcome to Orthosports Question for Physiotherapists April 2024. This month Dr John Negrine discusses the common condition of Gout. SAVE THE DATE: Orthosports Annual Orthopaedic Updates, Saturday, 9th
Distal Biceps Rupture
Welcome to Orthosports Question for Physiotherapists February 2024. This month Dr Doron Sher discusses management of distal biceps rupture. If you have a Question that you

Sport after Total Knee Replacement
Welcome to Orthosports Question for Physiotherapists, October 2023. This month Dr Doron Sher discusses return to sport after total knee replacement. REMINDER: Register your place for the Annual Orthopaedic Updates.

High Tibial Osteotomy and Uni Knee Replacement
Welcome to Orthosports Question for Physiotherapists, September 2023. This month Dr Doron Sher discusses the comparison of the High Tibial Osteotomy vs the Unicompartmental Knee Replacement. Register your
Achilles Tendon Ruptures
Welcome to Orthosports Question for Physiotherapists, August 2023. This month Dr John Negrine discusses Achilles Tendon Ruptures. Save the Date: Saturday, 4th November, 2023 Annual Orthopaedic Updates. Live

Lateral extra-articular tenodesis
Welcome to Orthosports Question for Physiotherapists, June 2023. This month Dr Michael Goldberg discusses lateral extra-articular tenodesis and why you would add this procedure to an ACL
Adding a Patch to Rotator Cuff Repairs
Welcome to Orthosports Question for Physiotherapists, May 2023. This month Dr Doron Sher discusses the use of a patch in Rotator Cuff Repairs. Save the Date: Saturday, 4th

Imaging for ACL Injury
Welcome to Orthosports Question for Physiotherapists, October 2022. This month Dr Doron Sher discusses imaging for a suspected ACL injury. Save the Date: Saturday, 12 November, 2022 Annual
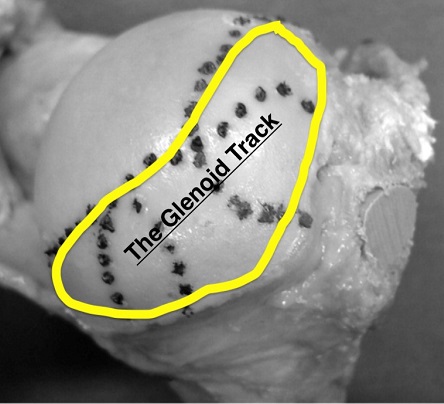
Glenoid Track and Shoulder Instability
Welcome to Orthosports Question for Physiotherapists August, 2022. This month Dr Doron Sher discusses a question on the glenoid track and shoulder instability. Please send your Questions

OSTEOCHONDRITIS DISSECANS
Welcome to Orthosports Question for Physiotherapists May, 2022. This month Dr Doron Sher discusses a question on treatment options for an OCD Lesion. Save the Date: Saturday,
Accessory Bones of the Foot and Ankle
Welcome to Question for Physiotherapists, April, 2022 This month Dr John Negrine discusses accessory bones of the foot and ankle. Please feel free to send your

Hypermobile Lateral Meniscus
Welcome to Question for Physiotherapists, March, 2022 This month Dr Michael Goldberg discusses the Hypermobile Lateral Meniscus. Please feel free to send your questions to

Imaging in Musculoskeletal assessment
Welcome to Question for Physiotherapists, February, 2022 This month Dr Paul Annett discusses Imaging inMusculo-skeletal Assessment. Please feel free to send your questions to education@orthosports.com.au Dr
Shoulder Injury related to vaccine administration
Welcome to Question for Physiotherapists, January, 2022 This month Dr Doron Sher discusses Shoulder Injury related to Vaccine administration. Please feel free to send your questions

Chondral Grafting in the knee
Welcome to Question for Physiotherapists, November 2021. This month Dr Doron Sher discusses Chondral Grafting in the knee.Please feel free to send your questions to education@orthosports.com.au CHONDRAL

Syndesmosis Fixation
Welcome to Question for Physiotherapists, October 2021. This month Dr Todd Gothelf discusses Syndesmosis fixation. Please feel free to send your questions to education@orthosports.com.au QUESTION I

Hip Precautions following Total Hip Replacement
Welcome to Question for Physiotherapists, September 2021. This month Dr Christopher Spelman discusses precautions after a Total Hip Replacement. Please feel free to send your questions
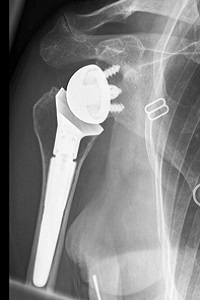
Reverse Shoulder Replacement Rehabilitation
Welcome to Question for Physiotherapists, August 2021. This month Dr Doron Sher discusses rehabilition after a Reverse Shoulder Replacement. Please feel free to send your questions
Chronic Scapholunate Ligament Rupture
Welcome to Question for Physios, July 2021. This month Dr Kwan Yeoh discusses the management of Complete Scapholunate Ligament Rupture. Please feel free to send your

Assessing Sports Injury
Welcome to Question for Physiotherapists June 2021. This month Dr Paul Annett presents an article on assessing a patient that presents with potentially more than a

Discoid Lateral Meniscus
Welcome to Question for Physiotherapists May 2021. This month Dr Doron Sher presents an article on a Discoid Lateral Meniscus. Please feel free to send

Cavo-Varus (High Arched) Feet
QUESTION | Why are high arched feet more interesting than flat feet? ANSWER | A 43 year old man presents with numbness on the outer

Surgical Treatment of Unstable Shoulder
QUESTION | | Surgical treatment of the unstable shoulder – How do you decide which patient gets what operation? We know that younger patients and those
Full Thickness Tear of Supraspinatus Tendon
QUESTION | My patient is a 67 year old female who has had pain during overhead activity (catching pain), going on for over 5 years.

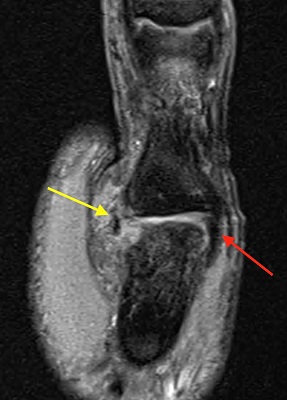
Medial Meniscal Root Tears
QUESTION I I have a patient in her 50s who has had a meniscus repair done. I thought that the studies showed no advantage when doing
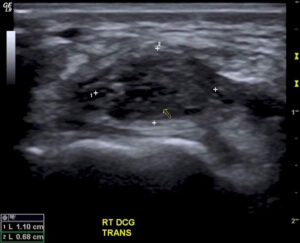
Wrist Ganglion & Carpal Instability
QUESTION| How Does a Wrist Ganglion relate to Carpal Instability? How is it best treated? ANSWER | A ganglion is a benign synovium-lined cystic collection of

Lumbar Stress Fractures
QUESTIONS | 1. What is rest in treatment of stress fracture? Walking only? Bike? Swim(in non-extended position)? What can you do? Or is it just not
Collateral Ligament Tear
QUESTION | WHEN DOES A COLLATERAL LIGAMENT TEAR OF THE THUMB NEED SURGERY? ANSWER | For the purposes of this question, I’m going to assume
Distal Biceps Rupture
QUESTION | I recently had a patient with a partial distal biceps rupture. Why was he offered surgery without trying non-operative management? ANSWER | Anatomy:

Hallux Rigidus
QUESTION | What are the best options for a 50 year old runner with Hallux Rigidus? ANSWER | A 50 year old runner with hallux
Previous Question for Physiotherapists:
| Dec-2020 | Wrist Ganglions | Dr Kwan Yeoh |
| Oct/Nov-2020 | Medial Meniscal Root Tears | Dr Doron Sher |
| Sep-2020 | Lumbar Stress Fractures | Dr Paul Annett |
| Aug-2020 | Frailty and Healthy Ageing | Dr John Best |
| Jul-2020 | Thumb – Collateral Ligament Tear | Dr Kwan Yeoh |
| Jun-2020 | Shoulder Instability | Dr Doron Sher |
| May-2020 | Hallux Rigidus | Dr John Negrine |
| Mar/Apr-2020 | Achilles Tendon Ruptures | Dr Todd Gothelf |
| Feb-2020 | Distal Biceps | Dr Doron Sher |
| Nov-2019 | Clavicle Fracture Internal Fixation | Dr Doron Sher |
| Oct-2019 | Femoracetabular Impingement (FAI) | Dr Paul Mason |
| Sep-2019 | Imaging for Acute ACL Injuries | Dr Doron Sher |
| Aug-2019 | Joint Relocation | Dr Paul Annett |
| Jul-2019 | Guyon canal surgery | Dr Kwan Yeoh |
| Jun-2019 | Whats new in ACL reconstruction 2019 | Dr Doron Sher |
| May-2019 | Cuneiform Fracture | Dr Todd Gothelf |
| Apr-2019 | Flexor Tendon Injuries | Dr Kwan Yeoh |
| Mar-2019 | Chronic Exertional Compartment Synd | Dr Paul Annett |
| Feb-2019 | Achilles Tendon Rupture | Dr John Negrine |
| Nov-2018 | Low Back Pain | Dr Paul Mason |
| Sep-2018 | Concussion part 2 | Dr John Best |
| Jul-2018 | Concussion part1 | Dr Paul Annett |
| Jun-2018 | Thessaly & McMurray Test | Dr Doron Sher |
| May-2018 | AC Joint | Dr Doron Sher |
| Apr-2018 | Arthritis of the fingers | Dr Kwan Yeoh |
| Feb-2018 | CLAVICLE fractures | Dr Doron Sher |
| Oct-2017 | ACL Grafts | Dr Doron Sher |
| Sep-2017 | Forefoot pain | Dr John Negrine |
| Aug-2017 | Wrist Ganglion | Dr Kwan Yeoh |
| Jul-2017 | Anterolateral Ligament Reconstruction | Dr Doron Sher |
| Jun-2017 | Scapholunate ligament | Dr Kwan Yeoh |
| Apr-2017 | Knee Brace – ACL Reconstruction | Dr Doron Sher |
| Mar-2017 | Sesamoid fractures | Dr Kwan Yeoh |
| Feb-2017 | Plantar Fasciitis | Dr Todd Gothelf |
| Nov-2016 | Sternoclavicular Joint | Dr Doron Sher |
| Oct-2016 | Proximal Humerus Fractures | Dr David Lieu |
| Sep-2016 | Wrist Fractures | Dr Kwan Yeoh |
| Aug-2016 | Patella Instability | Dr Doron Sher |
| Jul-2016 | Snowboarders ankle | Dr Todd Gothelf |
| May-2016 | Cortisone Injections | Dr Paul Annett |
| Apr-2016 | Shoulder Instability_1 | Dr Ivan Popoff |
| Mar-2016 | Exercise after TKR | Dr Doron Sher |
| Dec-2015 | Scaphoid OA | Dr Kwan Yeoh |
| Nov-2015 | Greater Tuberosity Fractures | Dr Doron Sher |
| Oct-2015 | Stress Fractures | Dr Paul Annett |
| Sep-2015 | Boxers Fractures | Dr Kwan Yeoh |
| Aug 2015 | Resistance Training | Dr John Best |
| July 2015 | LARS Ligament | Dr Ivan Popoff |
| Jun-2015 | Distal Biceps | Dr Doron Sher |
| May-2015 | Latarjet procedure | Dr Jerome Goldberg |
| Apr-2015 | TFCC Questions | Dr Kwan Yeoh |
| Mar-2015 | Acute Ankle Sprains | Dr Todd Gothelf |
| Nov-2014 | PRPP | Dr Paul Annett |
| Oct-2014 | Driving After Surgery | Dr Doron Sher |
| Sep-2014 | Distal Biceps Rupture | Dr Doron Sher |
| Aug-2014 | Ankle Sprain | Dr Todd Gothelf |
| Jun-2014 | Patella Dislocation | Dr Doron Sher |
| May-2014 | Shoulder Instability | Dr Todd Gothelf |
| Apr-2014 | De Quervains | Dr Kwan Yeoh |
| Mar-2014 | Acromio-clavicular joint injuries | Dr Todd Gothelf |
| Feb-2014 | Chronic Knee Pain | Dr Paul Annett |
| Dec-2013 | Foot and Ankle Questions | Dr John Negrine |
| Oct-2013 | Rotator Cuff Repair | Dr Todd Gothelf |
| Sep-2013 | ACL Reconstruction | Dr Doron Sher |
| Jul-2013 | Slipped Upper femoral epiphysis | Dr Rod Pattinson |
| May-2013 | Skiers thumb | Dr Kwan Yeoh |
| Apr-2013 | Bakers_Cyst | Dr Ivan Popoff |
| Mar-2013 | Tibial Osteotomy vs UKR | Dr Doron Sher |
| Feb-2013 | ALIF success rate | Dr Andreas Loefler |
| Jan-2013 | Lisfranc Injuries | Dr Todd Gothelf |
| Nov-2012 | Anterior Spinal Fusions | Dr Andreas Loefler |
| Oct-2012 | MCL Injuries | Dr Doron Sher |
| Sep-2012 | Compartment Syndrome | DrPaul Annett |
| Aug-2012 | Carpal tunnel | Dr Kwan Yeoh |
| July-2012 | Anterior Process Calcaneus Fx | Dr Todd Gothelf |
| Jun-2012 | Tenodesis vs Tenotomy | DrJeromeGoldberg |
| May-2012 | Osteoarthritis in the young active patient | Dr Doron Sher |
| Apr-2012 | Syndesmosis Sprain | Dr Todd Gothelf |
| Mar-2012 | Triangular Fiocartilage Injuries | Dr Kwan Yeoh |
| Jan-2012 | Shoulder Replacement Older Population | Dr Jerome Goldberg |
| Dec-2011 | Wrist Fracture | Dr Kwan Yeoh |
| Nov-2011 | Adductor Tendon Tear | Dr Paul Annett |
| Oct-2011 | Navicular Pain | Dr Todd Gothelf |
| Sep-2011 | OCD Lesion | Dr Doron Sher |
| Aug-2011 | Metal on Metal Hip Replacements | Dr Andreas Loefler |
| July-2011 | Femoral Neck Stress Fract (Pt 2) | Dr John Best |
| Jun-2011 | Femoral Neck Stress Fractures | Dr John Best |
| May-2011 | PCL Injury Part 2 | Dr Doron Sher |
| Apr-2011 | PCL Injury Part 1 | Dr DoronSher |
| Mar-2011 | Prolotherapy Autologous Blood Injections | DrPaul Annett |
| Feb-2011 | Shoulder Impingement | Dr Todd Gothelf |
| Dec-2010 | Does Chondral Grafting Work | DrDoron Sher |
| Nov-2010 | Shoulder Immobilisation-Dislocation | Dr Jerome Goldberg |
| Sep-2010 | SLAP Lesions Stable Shoulder | Dr ToddGothelf |
| Jul-2010 | Ankle Sprains | Dr Todd Gothelf |
| Jun-2010 | Dislocation After THR | Dr Peter Walker |
| May-2010 | Acupuncture Muscle Strength Programmes | Dr Paul Annett |
| April-2010 | Full Thickness Rotator Cuff Tears | Dr JeromeGoldberg |
| Mar-2010 | Skiing after TKR | Prof Warwick Bruce |
| Feb-2010 | Fractures of the Clavicle | Dr John Trantalis |
| Jan-2010 | Osteoarthritis of the Knee | Dr Doron Sher |
| Dec-2009 | Fifrth Metatarsal Fractures | Dr Todd Gothelf |
| Nov-2009 | Partial Rotator Cuff Tears | Dr Todd Gothelf |

